Binge eating disorder (BED) is a serious eating disorder characterized by recurrent episodes of binge eating, which involves consuming large amounts of food in a short period, often accompanied by feelings of loss of control, guilt, and shame. It's different from bulimia nervosa, as individuals with BED don't engage in purging or compensatory behaviors after bingeing.
BED can lead to physical and emotional health issues, such as weight gain, digestive problems, and decreased self-esteem. Treatment typically involves a combination of therapy, nutrition counseling, and support groups to address the emotional and psychological aspects of the disorder. Follow us here at Barbie dolls
Historical context
Early Years (1950s-1960s)
- Binge eating was first described as a symptom of depression and anxiety in the 1950s and 1960s.
- Researchers like Hilde Bruch and Albert Stunkard wrote about binge eating, but it wasn't yet recognized as a distinct disorder.
Emerging Recognition (1970s-1980s)
- In the 1970s and 1980s, researchers began to identify binge eating as a specific behavior, but it wasn't yet a formal diagnosis.
- Studies by researchers like Katherine Halmi and Craig Johnson explored binge eating concerning other eating disorders.
Provisional Diagnosis (1990s)
- In 1994, the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) introduced BED as a provisional diagnosis, requiring further research.
- This marked a significant turning point, as BED began to gain recognition as a distinct disorder.
Official Diagnosis (2000s)
- In 2013, the DSM-5 officially recognized BED as a distinct eating disorder, with specific diagnostic criteria.
- This recognition acknowledged BED's seriousness and prevalence and paved the way for more research and treatment development.
Current Understanding (2010s-present)
- Research continues to uncover the complexities of BED, including emotional regulation, trauma, and cultural factors.
- Treatment options have expanded, including cognitive-behavioral therapy (CBT), interpersonal psychotherapy (IPT), and medications.
- Advocacy efforts aim to reduce stigma and increase access to treatment, recognizing BED as a serious eating disorder.
Criteria
The diagnostic criteria for Binge Eating Disorder (BED) are outlined in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5). To diagnose BED, an individual must exhibit the following:
1. Recurring episodes of binge eating: Eating excessive food in a short period (e.g., within 2 hours) at least once a week for 3 months.
2. Characteristics of binge eating episodes:
- Eating rapidly
- Eating until uncomfortably full
- Eating alone due to embarrassment
3. Distress and impairment: Binge eating causes significant distress, and impairment in social, occupational, or other areas of life.
4. Not better explained by another eating disorder: BED is distinct from other eating disorders, such as bulimia nervosa or anorexia nervosa.
5. Severity specifier: BED severity is rated based on the frequency of binge eating episodes:
- Mild: 1-3 episodes/week
- Moderate: 4-7 episodes/week
- Severe: 8-13 episodes/week
- Extreme: 14 or more episodes/week
Signs and Symptoms
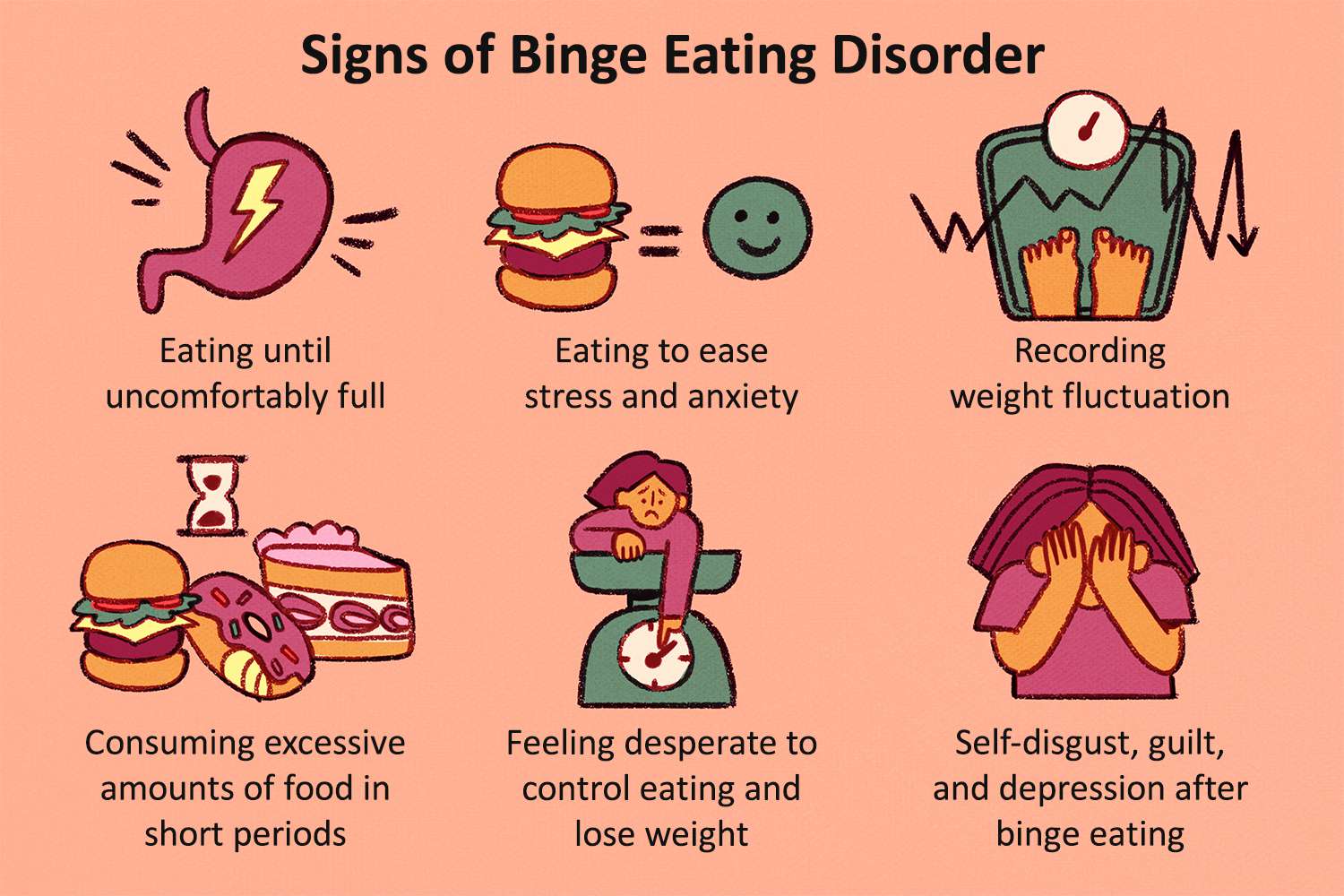
Signs and symptoms of Binge Eating Disorder (BED) that the naked eye can observe:
Physical Signs
1. Weight fluctuations: Noticeable weight gain or loss
2. Obesity: Visible excess body fat, particularly in the midsection
3. Poor grooming: Neglect of personal hygiene and appearance
4. Fatigue: Visible signs of exhaustion, such as dark circles under the eyes
5. Digestive issues: Visible discomfort, bloating, or abdominal pain
Behavioral Signs
1. Secretive eating: Eating in secret or hiding food wrappers
2. Rapid eating: Eating quickly, often without chewing properly
3. Overeating: Consuming large amounts of food in one sitting
4. Food avoidance: Avoiding social situations involving food
5. Emotional reactivity: Visible emotional distress, such as tears or irritability, after eating
Other Observable Signs
1. Food packaging: Excessive food packaging or wrappers in trash
2. Eating rituals: Engaging in unusual eating rituals, such as cutting food into small pieces
3. Social withdrawal: Avoiding social interactions or activities due to shame or guilt
4. Mood changes: Noticeable changes in mood, such as depression, anxiety, or irritability
5. Sleep disturbances: Visible signs of sleep deprivation or fatigue
Associative Features
1. Mental health conditions: BED often co-occurs with depression, anxiety disorders, substance use disorders, and other mental health conditions.
2. Emotional difficulties: Individuals with BED may struggle with emotional regulation, leading to feelings of guilt, shame, and self-criticism.
3. Body image concerns: BED is often linked to negative body image, low self-esteem, and weight-related concerns.
4. Dieting and weight cycling: BED can involve restrictive dieting, followed by binge eating, leading to weight fluctuations.
5. Gastrointestinal issues: BED may be associated with digestive problems, such as bloating, abdominal pain, and irritable bowel syndrome (IBS).
Prevalence and demographics
Prevalence
1. Lifetime prevalence: Approximately 3.5% of women and 2.0% of men in the United States will experience BED at some point in their lives.
2. 12-month prevalence: About 1.6% of adolescents (13-18 years old) and 2.8% of adults (18-65 years old) experience BED in a given year.
3. Estimated cases: BED affects an estimated 30 million people in the United States.
Demographics
1. Age: BED can occur at any age, but typically begins in adolescence (13-18 years old) or young adulthood (18-25 years old).
2. Sex: Women are more likely to develop BED than men, with a female-to-male ratio of approximately 2:1.
3. Ethnicity: BED affects individuals from diverse ethnic backgrounds, with a higher prevalence among African American and Hispanic populations.
4. Socioeconomic status: BED can occur across all socioeconomic levels, but may be more common among lower-income individuals.
5. Body weight: BED can affect individuals of any weight, but is more common among those with obesity (BMI ≥ 30).
Development and Course
Development
1. Early life experiences: Trauma, emotional neglect, or dysfunctional family dynamics may contribute to BED.
2. Dieting and weight concerns: Restrictive dieting, weight cycling, and negative body image can trigger binge eating.
3. Emotional regulation difficulties: Struggling to manage emotions, leading to binge eating as a coping mechanism.
4. Genetic predisposition: Genetic factors may play a role in BED, particularly in individuals with a family history of eating disorders.
Course
1. Onset: BED often begins in adolescence or young adulthood, but can start at any age.
2. Frequency and severity: Binge eating episodes may increase in frequency and severity over time.
3. Weight fluctuations: BED can lead to weight gain, obesity, or weight cycling.
4. Comorbidities: BED often co-occurs with other mental health conditions, such as depression, anxiety, or substance use disorders.
5. Chronicity: BED can be a chronic condition, with periods of remission and relapse.
6. Impact on daily life: BED can affect relationships, work, and overall quality of life.
Stages
1. Initial stage: Binge eating begins as an occasional behavior, often in response to emotional distress.
2. Maintenance stage: Binge eating becomes a regular behavior, often accompanied by weight gain and comorbidities.
Risk and Prognostic factors
Risk factors for BED
1. Genetic predisposition: Family history of eating disorders or obesity.
2. Dieting and weight concerns: Restrictive dieting, weight cycling, and negative body image.
3. Emotional difficulties: Difficulty managing emotions, trauma, or mental health conditions.
4. Sociocultural factors: Societal pressure to be thin, cultural emphasis on food and eating.
5. Personality traits: Perfectionism, impulsivity, and low self-esteem.
6. Co-occurring mental health conditions: Depression, anxiety, substance use disorders.
Prognostic factors for BED
1. Early intervention: Seeking treatment early in the course of the disorder.
2. Comorbidities: The presence of other mental health conditions can impact treatment outcomes.
3. Motivation for change: Individual's willingness to address binge eating behaviors.
4. Social support: A strong social support network can improve treatment outcomes.
5. Treatment type and duration: Effectiveness of treatment approach and length of treatment.
6. Relapse prevention strategies: There are strategies to prevent relapse, such as coping skills and support groups.
Good prognostic factors
1. Short duration of illness
2. Mild symptoms
3. High motivation for change
4. Strong social support
5. Effective treatment approach
Poor prognostic factors
1. Long duration of illness
2. Severe symptoms
3. Co-occurring mental health conditions
4. Lack of motivation for change
5. Ineffective treatment approach
Culture-related diagnostic issues
1. Cultural norms around food and eating: Different cultures have varying attitudes towards food, eating, and body shape, which can impact BED diagnosis.
2. Diverse presentations: BED may manifest differently across cultures, making diagnosis challenging.
3. Language barriers: Limited English proficiency can hinder accurate diagnosis and treatment.
4. Cultural stigma: Shame and stigma surrounding mental health issues, including BED, can lead to underreporting.
5. Different cultural values: Emphasis on thinness or food restriction may vary, influencing BED development and diagnosis.
Functional consequences
Functional consequences of BED:
1. Physical health problems: Obesity, metabolic issues, gastrointestinal problems, and sleep disturbances.
2. Mental health comorbidities: Depression, anxiety, substance use disorders, and low self-esteem.
3. Social and relationship difficulties: Strained relationships, social isolation, and feelings of guilt and shame.
4. Occupational and academic impairment: Reduced productivity, absenteeism, and decreased academic performance.
5. Economic consequences: Increased healthcare costs, lost productivity, and financial burdens.
6. Reduced quality of life: Impaired daily functioning, decreased enjoyment of activities, and overall reduced well-being.
7. Increased risk of other eating disorders: Development of other eating disorders, such as bulimia nervosa or anorexia nervosa.
8. Suicidal ideation and behavior: Increased risk of suicidal thoughts and actions.
The negative impact of BED on Life
1. Emotional Distress: Feelings of guilt, shame, anxiety, and depression.
2. Social Isolation: Avoiding social situations, relationships, and activities due to shame or fear of being judged.
3. Physical Health Problems: Obesity, metabolic issues, gastrointestinal problems, and sleep disturbances.
4. Mental Health Comorbidities: Co-occurring depression, anxiety, substance use disorders, and low self-esteem.
5. Occupational and Academic Impairment: Reduced productivity, absenteeism, and decreased academic performance.
6. Financial Burden: Increased healthcare costs, lost productivity, and financial strain.
7. Strained Relationships: Difficulty maintaining healthy relationships due to secrecy, shame, and emotional reactivity.
8. Loss of Enjoyment: Decreased participation in activities and hobbies due to feelings of guilt or shame.
9. Suicidal Ideation and Behavior: Increased risk of suicidal thoughts and actions.
10. Reduced Quality of Life: Impaired daily functioning, decreased overall well-being and reduced life satisfaction.
BED can also impact daily life in practical ways, such as:
- Difficulty maintaining a healthy weight
- Feeling self-conscious about eating in public
- Avoiding social gatherings or events involving food
- Spending excessive time thinking about food or eating
Differential Diagnosis
BED can be mistaken for other conditions, so it's essential to rule out:
1. Bulimia Nervosa: BED lacks purging behaviors.
2. Other Eating Disorders: Avoidant/Restrictive Food Intake Disorder (ARFID), Pica, Rumination Disorder.
3. Depression: BED is not just a symptom of depression, but a distinct disorder.
4. Anxiety Disorders: BED is not solely an anxiety disorder, although anxiety often co-occurs.
5. Substance Use Disorders: BED is not the same as substance abuse, although substance use may co-occur.
6. Gastrointestinal Disorders: BED is not solely a gastrointestinal issue, although GI symptoms may occur.
Comorbidity
BED often co-occurs with:
1. Depression (40-60% of individuals with BED)
2. Anxiety Disorders (30-50%)
3. Substance Use Disorders (20-30%)
4. Obsessive-Compulsive Disorder (OCD)
5. Post-Traumatic Stress Disorder (PTSD)
6. Attention Deficit Hyperactivity Disorder (ADHD)
7. Sleep Disorders
8. Chronic Pain
9. Gastrointestinal Disorders
10. Other Eating Disorders
Treatment and Management
Psychotherapies
1. Dialectical Behavior Therapy (DBT): Combines CBT with mindfulness techniques to manage emotions and behaviors.
2. Interpersonal Psychotherapy (IPT): Focuses on improving relationships and communication skills.
3. Family-Based Therapy: Involves family members in the treatment process.
Medications
1. Selective Serotonin Reuptake Inhibitors (SSRIs): Helps reduce binge eating frequency and severity.
2. Anti-Obesity Medications: May be prescribed for weight loss.
3. Mood Stabilizers: Can help manage co-occurring mood disorders.
Nutrition and Lifestyle Interventions
1. Nutrition Counseling: Helps individuals develop a balanced eating plan.
2. Meal Planning: Encourages regular, portion-controlled meals.
3. Stress Management: Techniques like meditation, yoga, or deep breathing can help manage stress.
Self-Help Strategies
1. Keeping a Food Diary: Tracks eating habits and identifies patterns.
2. Support Groups: Provide a sense of community and accountability.
3. Self-Compassion: Encourages self-kindness and understanding.
Treatment Settings
1. Outpatient: Individual or group therapy sessions.
2. Inpatient: Residential treatment programs for severe cases.
3. Online: Virtual therapy sessions and support groups.
Management
1. Regular Monitoring: Ongoing assessment and treatment adjustments.
2. Relapse Prevention: Strategies to maintain progress and prevent relapse.
3. Comorbidity Management: Addressing co-occurring mental health conditions.