Bulimia nervosa is an eating disorder with recurrent episodes of binge eating followed by compensatory behaviors to prevent weight gain. These behaviors may include vomiting, self-induced, excessive exercise, fasting, or misuse of laxatives or diuretics. Follow us here at Lily Collins
Criteria for Bulimia Nervosa
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the criteria for bulimia nervosa include:
- Recurrent episodes of binge eating: Consuming an abnormally large amount of food quickly, accompanied by a lack of control over eating.
- Recurrent inappropriate behaviors to prevent weight gain, such as vomiting, self-induced, excessive exercise, fasting, or misuse of laxatives or diuretics.
- The binge eating and compensatory behaviors occur, on average, at least once a week for three months.
- Self-evaluation is unduly influenced by body shape and weight.
Specifiers for Bulimia Nervosa
- Severity: Based on the frequency of weekly purging episodes.
- Mild: an average of one to three episodes per week.
- Moderate: an average of four to seven episodes per week.
- Severe: an average of eight to thirteen episodes per week.
- In partial remission: When criteria for bulimia nervosa have been met in the past but are not currently met, and binge eating, compensatory behaviors, and undue influence of weight on self-evaluation have occurred for less than three months.
- In full remission: When criteria for bulimia nervosa have been met in the past but are not currently met, and no criteria have been met for the past 12 months.
Understanding the criteria and specifiers for bulimia nervosa is essential for accurate diagnosis and treatment planning.
Signs and Symptoms
Binge Eating

- Consuming abnormally large amounts of food in a short time.
- Didn't Feel any control over eating during the binge.
- Eating rapidly and without paying attention to hunger cues.
Compensatory Behaviors
- Self-induced vomiting
- Excessive exercise
- Fasting or strict dieting
- Misuse of laxatives, diuretics, or enemas
Other Signs and Symptoms
- Fluctuating weight, often within a normal range.
- Swollen salivary glands.
- Electrolyte imbalances.
- Dehydration.
- Withdrawal from social activities.
- Low self-esteem and body dissatisfaction.
It's important to note that people with bulimia may go to great lengths to hide their eating disorder, making it difficult to detect.
Prevalence and Demographics
Prevalence
- Bulimia nervosa is a relatively common eating disorder, particularly among young women.
- Exact prevalence rates vary across studies and populations, but it is estimated to affect approximately 1-3% of young women.
- The prevalence among men is significantly lower but increasing.
Demographics
- Age of onset: Typically begins in adolescence or young adulthood.
- Gender: While bulimia nervosa is more prevalent in females, it also affects males.
- Socioeconomic status: This can occur in individuals from all socioeconomic backgrounds.
- Cultural factors: The prevalence and expression of bulimia nervosa can vary across cultures.
Development and Course
Development
While the exact causes are complex and not fully understood, several factors may contribute to its development, including:
- Biological factors: Genetic predisposition, neurotransmitter imbalances.
- Psychological factors: Low self-esteem, body dissatisfaction, perfectionism.
- Social and cultural factors: Media portrayal of ideal body image, dieting trends.
Course
The course of bulimia nervosa can vary widely among individuals. Some people may experience chronic symptoms, while others may have periods of remission and relapse.
- Chronic course: Characterized by persistent binge eating and compensatory behaviors.
- Episodic course: Alternating periods of symptomatic and asymptomatic phases.
- Recovery: With appropriate treatment, many individuals can achieve significant improvement and recovery.
Risk and Prognostic Factors
Risk Factors
Several factors can increase the risk of developing bulimia nervosa:
- Genetic predisposition: Having a family history of eating disorders or other mental health conditions.
- Psychological factors: Low self-esteem, perfectionism, body dissatisfaction, and impulsivity.
- Environmental factors: Societal pressure to be thin, dieting, and exposure to media promoting unrealistic body images.
- Other mental health conditions: Comorbid disorders such as depression, anxiety, or substance abuse.
- Personality traits: Individuals with certain personality traits, like novelty-seeking or impulsivity, may be at higher risk.
Prognostic Factors
Factors that can influence the course and outcome of bulimia nervosa include:
- Early intervention: Seeking treatment early in the course of the disorder improves prognosis.
- Severity of symptoms: The frequency and intensity of binge eating and compensatory behaviors impact treatment outcomes.
- Comorbid conditions: The presence of other mental health disorders can complicate treatment.
- Social support: A strong support system can facilitate recovery.
- Treatment adherence: Consistent engagement in treatment is crucial for long-term success.
Culture-Related Diagnostic Issues
- Cultural ideals of beauty: Societal pressures to conform to unrealistic body standards can contribute to the development of bulimia nervosa. Different cultures have varying beauty ideals, which can influence the prevalence and presentation of the disorder.
- Stigma: Cultural stigma associated with eating disorders can prevent individuals from seeking help and treatment.
- Food-related cultural practices: Certain cultural practices or dietary restrictions may be misinterpreted as disordered eating behaviors.
Gender-Related Diagnostic Issues
- Gender stereotypes: Bulimia nervosa is often perceived as a primarily female disorder, leading to underdiagnosis in males.
- Symptom presentation: There may be differences in symptom presentation between males and females, such as compensatory behaviors.
- Treatment-seeking behavior: Males may be less likely to seek help due to societal expectations and stigma.
Diagnostic Markers
Diagnostic markers for bulimia nervosa focus on the cyclical pattern of binge eating and compensatory behaviors.
- Binge eating episodes: Recurrent episodes of consuming large amounts of food in a short time, accompanied by a sense of lack of control.
- Compensatory behaviors: Regular engagement in self-induced vomiting, excessive exercise, fasting, or misuse of laxatives or diuretics.
- Body image disturbance: Overvaluation of body shape and weight, leading to negative self-evaluation.
- Electrolyte imbalances: Due to frequent vomiting or misuse of laxatives.
- Dental problems: Erosion of tooth enamel from stomach acid.
- Swollen salivary glands: As a result of frequent vomiting.
Causes
The exact cause of bulimia nervosa is unknown, but it's believed to be a complex interaction of biological, psychological, and environmental factors.
Biological Factors
- Genetics: Having a family history of eating disorders or other mental health conditions can increase the risk.
- Brain chemistry: Imbalances in neurotransmitters may contribute to the development of bulimia.
Psychological Factors
- Low self-esteem: Negative body image and feelings of inadequacy.
- Perfectionism: Striving for unattainable standards of excellence.
- Difficulty controlling emotions: Using food to cope with negative emotions.
- Distorted body image: Perceiving one's body as larger than it is.
Environmental Factors
- Societal pressure: Idealization of thinness in media and culture.
- Dieting: Restrictive diets can trigger binge eating.
- Trauma: A history of physical or emotional abuse can increase the risk.
- Family dynamics: Dysfunctional family relationships or communication patterns.
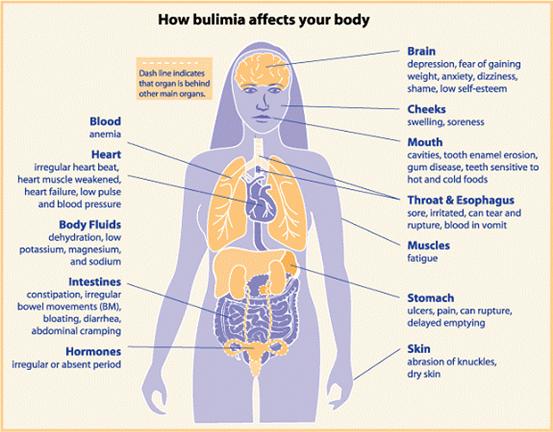
Functional Consequences
Bulimia nervosa can have significant functional consequences affecting various aspects of life:
- Physical health: Electrolyte imbalances, dental problems, gastrointestinal issues, and nutritional deficiencies.
- Psychological health: Depression, anxiety, low self-esteem, and body dissatisfaction.
- Social functioning: Isolation, strained relationships, and difficulty maintaining social connections.
- Occupational or academic difficulties: Impaired concentration, reduced productivity, and absenteeism.
- Financial difficulties: Spending on food, diet products, or dental care.
Suicidal Risk
Individuals with bulimia nervosa are at an increased risk of suicide compared to the general population. Factors contributing to this risk include:
- Depression: Often co-occurs with bulimia nervosa.
- Low self-esteem: Negative self-evaluation can lead to feelings of hopelessness.
- Impulsivity: Associated with binge eating and compensatory behaviors.
Negative Impacts of Bulimia Nervosa on Life
Bulimia nervosa has significant negative impacts on various aspects of a person's life:
Physical Health Consequences
- Electrolyte imbalances: Can lead to heart arrhythmias, seizures, and even death.
- Dental problems: Tooth erosion due to stomach acid.
- Gastrointestinal issues: Inflammation of the esophagus, stomach, and intestines.
- Dehydration: This can lead to kidney problems and other health complications.
Psychological Consequences
- Low self-esteem: Negative body image and feelings of inadequacy.
- Depression and anxiety: Common comorbidities that can worsen symptoms.
- Obsessive thoughts: Constant preoccupation with food, weight, and body shape.
Social Consequences
- Isolation: Withdrawal from social activities due to shame and embarrassment.
- Strained relationships: Difficulty maintaining relationships due to mood swings, secrecy, and unpredictable behavior.
- Academic or occupational difficulties: Impaired concentration, reduced productivity, and absenteeism.
Financial Consequences
- Spending on food, diet products, and dental care.
- Potential loss of income due to illness or inability to work.
Differential Diagnosis
Differential diagnosis involves distinguishing bulimia nervosa from other conditions that may present with similar symptoms. It's crucial for accurate diagnosis and appropriate treatment.
Conditions to consider
- Anorexia nervosa: Distinguished by persistent restriction of energy intake leading to significantly low body weight.
- Binge eating disorder: Involves recurrent episodes of binge eating without compensatory behaviors.
- Avoidant/restrictive food intake disorder: Characterized by persistent failure to meet appropriate nutritional needs without fear of weight gain.
- Major depressive disorder: This can include overeating or decreased appetite.
- Borderline personality disorder: May involve emotional instability and impulsive behaviors, including overeating.
- Substance abuse: Can contribute to binge eating or disordered eating patterns.
- Medical conditions: Gastrointestinal disorders or metabolic conditions can cause symptoms that mimic bulimia nervosa.
Comorbidity
Bulimia nervosa often co-occurs with other mental health conditions, which can complicate treatment and recovery. Common comorbidities include:
- Mood disorders: Depression, bipolar disorder
- Anxiety disorders: Generalized anxiety disorder, panic disorder, social anxiety disorder
- Substance abuse: Alcohol, drugs
- Personality disorders: Borderline personality disorder
- Eating disorders: Anorexia nervosa or binge eating disorder
Treatment and Management
Treatment of Bulimia Nervosa
Treatment for bulimia nervosa typically involves a combination of therapy and medication.
- Psychotherapy: Cognitive-behavioral therapy (CBT) is the most effective treatment for bulimia nervosa. It helps individuals identify and change negative thought patterns and behaviors. Other forms of therapy, such as interpersonal therapy and dialectical behavior therapy, may also be helpful.
- Medication: Antidepressants can be used to address mood symptoms and reduce binge eating and purging behaviors. However, they are not a primary treatment for bulimia nervosa.
- Nutritional counseling: A registered dietitian can guide healthy eating habits and meal planning.
Management of Bulimia Nervosa
Managing bulimia nervosa is an ongoing process that requires patience and support.
- Regular medical check-ups: To monitor physical health and address any nutritional deficiencies.
- Support groups: Connecting with others who have similar experiences can be beneficial.
- Family involvement: Involving family members in the treatment process can be supportive.
- Relapse prevention: Developing strategies to cope with triggers and prevent relapse.
- Long-term care: Ongoing support and monitoring are essential for maintaining recovery.