Dissociative Identity Disorder (DID), commonly known as Multiple Personality Disorder, is a mental health condition characterized by the presence of two or more distinct personality states. These distinct identities, often called "alters," control people's behavior at different times.
DID is believed to be a coping mechanism for severe trauma, typically experienced in childhood. It's a way for the mind to compartmentalize and dissociate from overwhelming experiences. Follow us here at "Saltburn"
Significant memory gaps mark the disorder, as information and experiences are often compartmentalized within the different identities. Individuals with DID may experience changes in their sense of self, perception of their surroundings, and even physical symptoms.
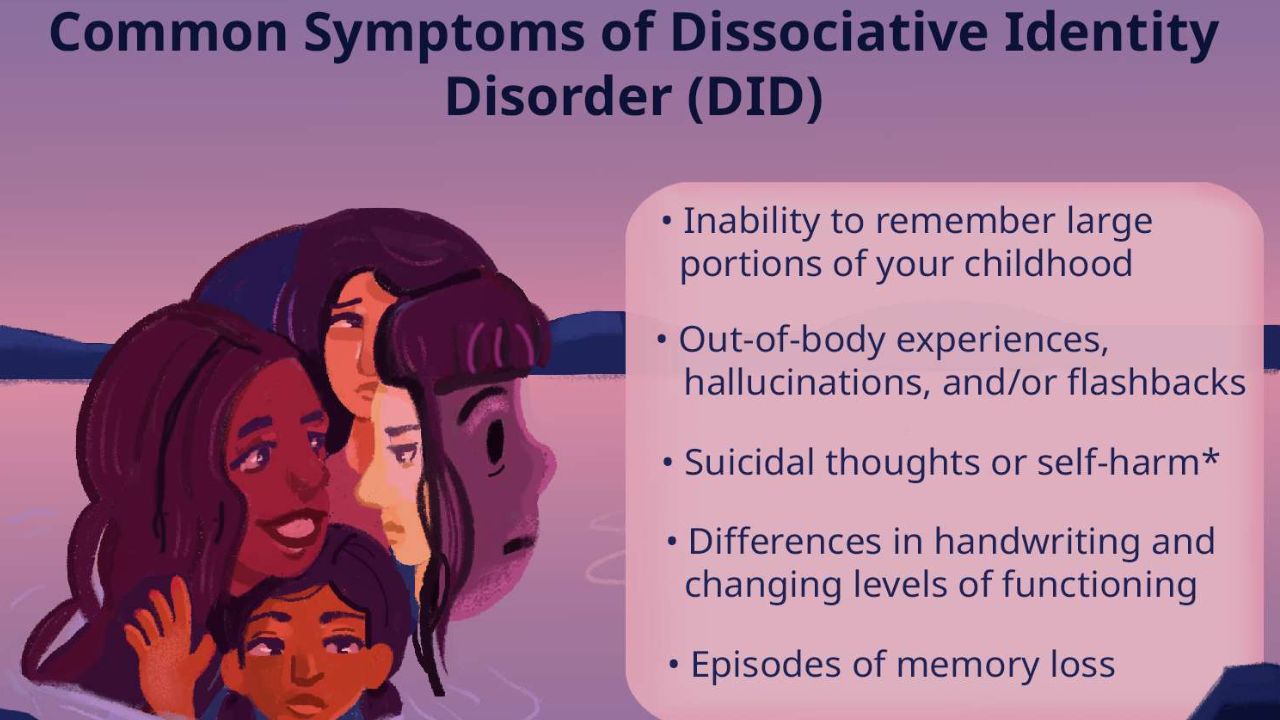
Signs and Symptoms
Dissociative Identity Disorder (DID) is characterized by the presence of two or more distinct personality states, often referred to as "alters." These alters can have different names, ages, genders, and even physical characteristics.
Core Symptoms
- Presence of two or more distinct identities or personality states: Each identity has its unique patterns of behavior, memory, and self-perception.
- Amnesia: Gaps in memory for everyday events, personal information, and traumatic events.
- Switching: The shifting between different identities, which can occur suddenly and involuntarily.
Additional Symptoms
- Derealization: Feeling detached from one's surroundings.
- Mood swings: Rapid and unpredictable changes in mood.
- Self-harm: Some individuals with DID engage in self-harm as a way to cope with emotional pain.
- Suicidal thoughts and behaviors: Increased risk of suicide due to the overwhelming nature of the condition.
- Substance abuse: May be used as a coping mechanism.
- Physical symptoms: Headaches, chronic pain, and other physical ailments often accompany DID.
It's important to note that DID is a complex disorder, and symptoms can vary widely from person to person.
Impact of DID on Life
Dissociative Identity Disorder (DID) profoundly impacts various aspects of a person's life. The core of the disorder involves the fragmentation of identity, which can lead to a cascade of challenges.
Interpersonal Relationships
- Difficulty building trust: The unpredictable nature of DID can make it challenging to establish and maintain trust in relationships.
- Communication breakdowns: Different alters may have different communication styles, leading to misunderstandings and conflicts.
- Isolation: The fear of being misunderstood or rejected often leads to social withdrawal.
Occupational and Academic Functioning
- Difficulty maintaining employment: Dissociation, memory gaps, and inconsistent behavior can hinder job performance.
- Academic struggles: Concentration difficulties, memory problems, and emotional instability can impact academic achievement.
Mental and Physical Health
- Increased risk of self-harm and suicide: The intense emotional pain associated with DID can lead to self-destructive behaviors.
- Physical health problems: Dissociation can impact sleep, eating habits, and overall physical well-being.
Daily Living
- Memory gaps: Difficulty remembering events, appointments, or personal information.
- Identity confusion: Uncertainty about one's own identity and sense of self.
- Financial difficulties: Challenges with managing money due to memory problems or impulsive spending.
Legal Issues
- Criminal behavior: Dissociative states can lead to actions that the individual may not remember.
- Child custody challenges: The complexities of DID can impact child custody arrangements.

Prevalence and Demographics
Prevalence
Determining the exact prevalence of Dissociative Identity Disorder (DID) is challenging due to several factors:
- Underreporting: Many cases go undiagnosed or misdiagnosed.
- Stigma: The condition is often misunderstood and stigmatized, leading to reluctance to seek help.
- Diagnostic criteria: Changes in diagnostic criteria over time can affect prevalence rates.
That said, estimates vary widely. Some studies suggest:
- General population: 1-3%
- Psychiatric inpatient settings: 2-5%
- Psychiatric outpatient settings: 2-3%
It's important to note that these are estimates and the actual prevalence might be higher.
Demographics
- Gender: DID is diagnosed significantly more often in women than in men.
- Age of onset: The disorder typically begins in childhood, often as a response to severe trauma.
- Comorbidity: DID often co-occurs with other mental health conditions, such as depression, anxiety, and substance abuse.
- Trauma history: A history of severe childhood trauma, especially physical, emotional, or sexual abuse, is strongly associated with DID.
It's essential to remember that these are general trends and individual experiences can vary widely. DID is a complex condition that requires careful diagnosis and treatment.

Development and Course
Development
Dissociative Identity Disorder (DID) is a complex mental health condition that typically develops as a coping mechanism in response to severe, prolonged childhood trauma.
- Childhood Trauma: Overwhelming experiences of abuse, neglect, or other forms of trauma can disrupt a child's developing sense of self. To cope with the unbearable pain, the mind may compartmentalize the trauma into different personality states.
- Dissociation: This process of compartmentalization is known as dissociation, where the mind separates painful memories and experiences from conscious awareness. Over time, these dissociated parts of the self may develop into distinct personalities or alter.
- Alter Formation: Each alter develops unique coping mechanisms, memories, and behaviors to manage specific aspects of the trauma. This creates a complex system of personalities within one individual.
Course
The course of DID is often chronic, with symptoms fluctuating in severity over time. Factors such as stress, trauma re-exposure, and treatment can influence the expression of the disorder.
- Chronic Condition: DID is generally considered a lifelong condition, requiring ongoing management and support.
- Fluctuating Symptoms: The frequency and intensity of dissociative symptoms can vary. Periods of relative stability may be interspersed with periods of increased distress or symptom severity.
- Impact on Functioning: The disorder can significantly impair a person's ability to function in various life areas, including relationships, work, and social interactions.
- Treatment Response: With appropriate treatment, individuals with DID can learn to manage their symptoms, reduce the impact of the disorder, and improve overall quality of life.
Risks and Prognostic Factors
Risks Associated with DID
Individuals with DID face several significant risks, including:
- Self-harm and suicide: These are alarmingly high among individuals with DID. The intense emotional pain associated with the disorder can lead to self-destructive behaviors.
- Relationship difficulties: DID can significantly impact interpersonal relationships due to the nature of the disorder and the challenges it presents.
- Occupational and academic difficulties: The symptoms of DID can interfere with daily functioning, making it difficult to maintain employment or pursue education.
- Re-traumatization: Due to the nature of the disorder, individuals with DID are at increased risk of experiencing further trauma.
Prognostic Factors
Prognostic factors are elements that can influence the outcome of a condition. While DID is a complex disorder with a chronic course, several factors can impact prognosis:
- Early intervention: Early identification and treatment can improve outcomes.
- Treatment adherence: Consistent engagement in therapy is crucial for progress.
- Support system: A strong support network can provide encouragement and assistance.
- Severity of trauma: The nature and extent of childhood trauma can influence the severity and complexity of DID.
- Comorbid conditions: The presence of other mental health disorders can complicate treatment and recovery.
Culture and Gender-Related Diagnostic Issues in DID
Cultural Factors
Cultural beliefs and practices can significantly impact the presentation and diagnosis of Dissociative Identity Disorder (DID).
- Cultural Explanations of Distress: Some cultures may attribute dissociative symptoms to possession, spirit possession, or other culturally specific phenomena, leading to misdiagnosis or delayed treatment.
- Stigma: The stigma associated with mental illness, particularly dissociative disorders, can vary across cultures. This can influence the willingness of individuals to seek help or disclose symptoms.
- Trauma and Culture: Cultural factors can shape the types of trauma experienced and how individuals cope with trauma, potentially influencing the development of DID.
Gender Factors
Gender plays a crucial role in the diagnosis and understanding of DID.
- Overrepresentation of Women: DID is more commonly diagnosed in women. However, it's essential to consider that this could be due to several factors, including reporting biases, societal expectations, and differences in trauma exposure.
- Gender Roles and Expression: Cultural expectations about gender roles can influence the expression of DID symptoms. For example, men may be less likely to report dissociative symptoms due to societal pressures to be strong and independent.
- Trauma and Gender: Women are more likely to experience certain types of trauma, such as sexual abuse, which are associated with DID. However, men can also experience severe trauma and develop DID.
Diagnostic Challenges
These cultural and gender-related factors can contribute to several diagnostic challenges:
- Overdiagnosis or Underdiagnosis: Misunderstanding of cultural expressions of distress or gender-related biases can lead to either overdiagnosis or underdiagnosis of DID.
- Difficulty in Assessment: Accurately assessing DID requires a deep understanding of the individual's cultural background and experiences.
- Treatment Challenges: Cultural and gender-related factors can impact the effectiveness of treatment, as it's essential to consider these factors when developing a treatment plan.
Functional Consequences
Dissociative Identity Disorder (DID) can have a significant impact on a person's ability to function in daily life. Here are some of the common functional consequences of DID:
Difficulties in maintaining relationships
The unpredictable nature of DID symptoms can strain relationships with family, friends, and romantic partners. Dissociation can make it difficult to trust others or feel close to them. Alters may have different relationships with different people, which can be confusing for those who don't understand DID.
Challenges in employment and education
Dissociation and amnesia can interfere with work performance and academic success. People with DID may have difficulty concentrating, following through on tasks, or remembering important information. They may also miss work or school due to dissociative episodes.
Self-harm and suicidal behaviors
DID is associated with an increased risk of self-harm and suicide due to the overwhelming emotional pain that people with DID experience. Dissociation can be a way of coping with this pain, but it can also lead to self-destructive behaviors.
Impaired daily functioning
Dissociation can disrupt daily routines, making it difficult to manage tasks, appointments, and finances. People with DID may forget to take care of basic needs, such as eating and sleeping. They may also have difficulty managing their time or staying organized.
Difficulties with self-care
Taking care of oneself can be challenging due to dissociation and amnesia. People with DID may forget to take their medications, eat healthy foods, or exercise. They may also neglect their hygiene or appearance.
Substance abuse
Individuals with DID may turn to substances to cope with the emotional distress associated with the disorder. Substance abuse can worsen DID making it more difficult to function in daily life.
Legal problems
Dissociative episodes can lead to risky behaviors or gaps in memory that could result in legal problems. For example, a person with DID may commit a crime while dissociated and have no memory of doing so.
Differential Diagnosis
Differential diagnosis involves considering other possible conditions that might explain a patient's symptoms. It's crucial to distinguish DID from other disorders to ensure accurate diagnosis and appropriate treatment.
Here are some conditions often considered in the differential diagnosis of DID:
Psychiatric Disorders
- Borderline Personality Disorder (BPD) is often considered the most common differential diagnosis due to overlapping symptoms like impulsivity, emotional instability, and self-harm.
- Schizophrenia and other psychotic disorders: Delusions or hallucinations can be mistaken for communication with different alters.
- Bipolar Disorder: Rapid mood swings and dissociative-like symptoms can occur during manic or depressive episodes.
- Post-Traumatic Stress Disorder (PTSD): Both DID and PTSD involve trauma, but DID is characterized by distinct personality states, while PTSD focuses on re-experiencing trauma.
- Somatic Symptom Disorder: Physical symptoms without a clear medical explanation can sometimes mimic dissociative symptoms.
- Factitious Disorder and Malingering: These conditions involve intentional falsification of symptoms, which must be ruled out.
Other Conditions
- Epilepsy: Some seizure types can mimic dissociative symptoms, such as automatisms or altered states of consciousness.
- Substance-Induced Disorders: Substance abuse can induce symptoms resembling DID.
- General Medical Conditions: Certain medical conditions can cause symptoms that mimic dissociative disorders.
Comorbidity
Dissociative Identity Disorder (DID) frequently co-occurs with other mental health conditions.
Borderline Personality Disorder (BPD)
BPD is characterized by emotional instability, impulsivity, and intense interpersonal relationships
Schizophrenia and other psychotic disorders
These disorders involve hallucinations or delusions that can be mistaken for communication with different alters.
Bipolar Disorder
Rapid mood swings and dissociative-like symptoms can occur during manic or depressive episodes.
Post-Traumatic Stress Disorder (PTSD)
Both DID and PTSD involve trauma, but DID is characterized by distinct personality states, while PTSD focuses on re-experiencing trauma.
Somatic Symptom Disorder
Physical symptoms without a clear medical explanation can sometimes mimic dissociative symptoms.
Factitious Disorder and Malingering
These conditions involve intentional falsification of symptoms, which must be ruled out.
Depression
Depression is a common comorbidity of DID, and people with DID may experience symptoms of intense sadness, hopelessness, and worthlessness.
Anxiety disorders
Anxiety disorders, such as generalized anxiety disorder or social anxiety disorder, frequently co-occur with DID.
Substance use disorders
People with DID may turn to substances to cope with the emotional distress associated with the disorder. Substance can worsen DID symptoms and make it more difficult to function in daily life.
Treatment and Management
Treatment for DID is primarily focused on psychotherapy, as there is no specific medication for the disorder itself. However, medications can be used to manage associated symptoms like depression, anxiety, or sleep disturbances.
Psychotherapy
- Trauma-focused therapy: This is the cornerstone of treatment. It helps individuals process and understand the traumatic experiences that led to the development of DID.
- Dialectical behavioral therapy (DBT): This therapy focuses on emotional regulation, distress tolerance, interpersonal effectiveness, and mindfulness.
- Psychodynamic therapy: This therapy explores unconscious conflicts and patterns of behavior.
Medication
While there's no specific medication for DID, medications can help manage associated symptoms:
- Antidepressants: For depression and anxiety.
- Mood stabilizers: For mood swings and irritability.
- Antipsychotics: In some cases, to manage severe symptoms.
Other Treatments
- Support groups: Connecting with others who have DID can provide valuable support and coping strategies.
- Education: Understanding DID is crucial for both the individual and their support system.
- Safety planning: Developing a safety plan can help manage crises and reduce the risk of self-harm.