Elimination Disorders are a group of psychological disorders characterized by the intentional elimination of bodily waste in inappropriate places, such as outside of a toilet. These disorders are often seen in children, but can also occur in adults. Follow us here at Building Muscle Tag
There are two types of Elimination Disorders:
1. Enuresis: Also known as bedwetting, this is the repeated urination in inappropriate places, such as in bed or on clothing.
2. Encopresis: Also known as fecal soiling, this is the intentional or involuntary passing of feces in inappropriate places, such as in clothing or on the floor.
Enuresis
Enuresis, also known as bedwetting, is a common elimination disorder characterized by repeated urination in inappropriate places, such as in bed or on clothing. It is a complex condition that affects millions of children and adults worldwide.
Definition
Enuresis is defined as the involuntary discharge of urine during sleep, typically occurring in children aged 5 and above in adults.
Diagnostic Criteria
A. Repeated urination in inappropriate places (e.g., bed, clothing), whether intentional or involuntary.
B. At least two such events occur per week for at least 3 months, or the presence of significant distress or impairment in social, occupational, or other areas of functioning.
C. The behavior is not due to a general medical condition (e.g., urinary tract infection, diabetes) or a neurological disorder (e.g., spinal cord injury).
D. The behavior is not better explained by another mental disorder (e.g., intellectual disability, autism spectrum disorder).
Subtypes of Enuresis
1. Nocturnal Enuresis: Bedwetting that occurs at night, typically during deep sleep.
2. Diurnal Enuresis: Urination in inappropriate places during the day.
3. Mixed Nocturnal and Diurnal Enuresis: A combination of both nocturnal and diurnal enuresis.
4. Primary Enuresis: The individual has never achieved consistent bladder control.
5. Secondary Enuresis: The individual has previously achieved bladder control, but has since lost it.
Severity Specifiers
- Mild: Fewer than 2 episodes per week.
- Moderate: 2-4 episodes per week.
- Severe: 5 or more episodes per week.
Associative Features
1. Genetic predisposition: Family history of enuresis.
2. Constipation: Bowel habits and constipation can contribute to enuresis.
3. Emotional distress: Anxiety, depression, trauma.
4. Developmental delays: Delays in bladder control, and toilet training.
Prevalence and demographics
Prevalence
1. Nocturnal Enuresis: Affects approximately 5-10% of children aged 5-10 years.
2. Diurnal Enuresis: Affects approximately 2-5% of children aged 5-10 years.
3. Mixed Nocturnal and Diurnal Enuresis: Affects approximately 1-3% of children aged 5-10 years.
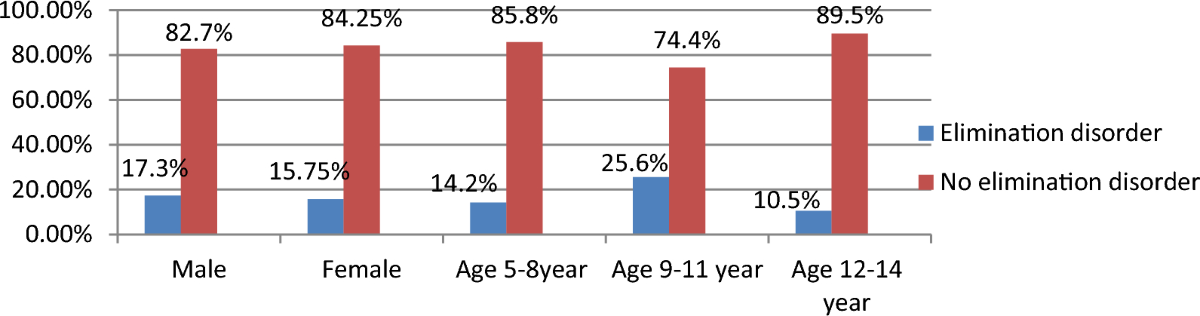
Demographics
1. Age: Enuresis is most common in children aged 5-10 years.
2. Sex: Boys are more likely to experience enuresis than girls.
3. Socioeconomic status: Enuresis is more common in lower socioeconomic groups.
4. Family history: Individuals with a family history of enuresis are more likely to experience it.
5. Comorbidities: Enuresis often co-occurs with other conditions, such as ADHD, and ASD.
Development and Course
Development
1. Infancy and Toddlerhood: Enuresis is a normal part of development, as infants and toddlers lack bladder control.
2. Early Childhood: Most children achieve nighttime bladder control by age 3-4 and daytime control by age 4-5.
3. School-Age Children: Enuresis can persist in some children, often due to underlying medical or psychological issues.
Course
1. Primary Enuresis: The child has never achieved consistent bladder control.
2. Secondary Enuresis: The child has previously achieved bladder control, but has since lost it.
3. Nocturnal Enuresis: Bedwetting that occurs at night, often due to:
- Deep sleep patterns
- Small bladder capacity
- Hormonal imbalances
- Sleep apnea
4. Diurnal Enuresis: Urination in inappropriate places during the day, often due to:
- Attention deficit hyperactivity disorder (ADHD)
- Anxiety or stress
- Constipation
- Urinary tract infections
5. Mixed Nocturnal and Diurnal Enuresis: A combination of both nocturnal and diurnal enuresis.
Factors Influencing Course
1. Genetics: Family history of enuresis
2. Medical Conditions: Constipation, urinary tract infections, diabetes, or neurological disorders
3. Psychological Factors: Anxiety, stress, or trauma
4. Environmental Factors: Changes in routine, stress, or sleep patterns
5. Developmental Delays: Delayed bladder control or cognitive development
Age-Related Changes
1. Preschool-Age Children: Enuresis is more common and often resolves with age.
2. School-age children: Enuresis can persist and may be more embarrassing and distressing.
3. Adolescents: Enuresis can be more stigmatizing and may impact self-esteem.
4. Adults: Enuresis can be a persistent problem, often requiring medical evaluation and treatment.
Risk(Causes) and Prognostic factor
Risk Factors/Causes for Enuresis
1. Genetic predisposition: A family history of enuresis increases the risk.
2. Neurodevelopmental disorders: Conditions like ADHD, autism spectrum disorder, and intellectual disability.
3. Sleep disorders: Sleep apnea, restless leg syndrome, and insomnia.
4. Urinary tract abnormalities: Urinary tract infections, bladder problems, or kidney issues.
5. Constipation: Constipation can contribute to bladder control problems.
6. Psychological factors: Stress, anxiety, and emotional distress.
7. Environmental factors: Changes in routine, moving to a new home, or starting school.
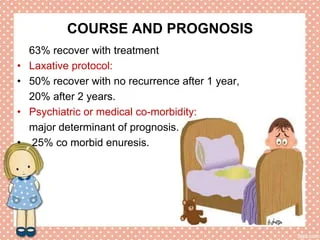
Prognostic Factors for Enuresis
1. Age: Enuresis that persists beyond age 5-6 is more likely to be a chronic condition.
2. Frequency and severity: More frequent and severe episodes indicate a poorer prognosis.
3. Duration: Longer duration of enuresis is associated with a poorer prognosis.
4. Comorbidities: The presence of other conditions, such as ADHD or sleep disorders, can impact treatment outcomes.
5. Treatment response: Response to initial treatment can predict long-term outcomes.
6. Family dynamics: A supportive family environment and parental involvement can improve treatment outcomes.
7. Child's motivation: Child's willingness to participate in treatment and take responsibility for bladder control.
Poor Prognostic Factors
1. Severe enuresis: Frequent and severe episodes.
2. Long duration: Enuresis that persists for more than 2-3 years.
3. Comorbidities: Presence of multiple comorbid conditions.
4. Treatment resistance: Failure to respond to multiple treatments.
5. Family conflict: High levels of family conflict and stress.
Good Prognostic Factors
1. Mild enuresis: Infrequent and mild episodes.
2. Short duration: Enuresis that has been present for less than 2 years.
Culture-Related Diagnostic Issues
1. Cultural norms around toilet training: Different cultures have varying expectations around toilet training, which can impact diagnosis.
2. Stigma and shame: Enuresis may be stigmatized in some cultures, leading to underreporting or delayed seeking of treatment.
3. Traditional practices: Certain cultural practices, such as delayed toilet training or the use of diapers, may be misinterpreted as enuresis.
4. Language barriers: Limited English proficiency can hinder accurate diagnosis and treatment.
5. Diverse definitions of "normal": Cultural differences in what is considered "normal" bladder control can affect diagnosis.
Examples
- In some African cultures, children are not expected to achieve bladder control until age 5-6.
- In some Asian cultures, toilet training is delayed until age 3-4.
- In some Indigenous cultures, enuresis is not seen as a problem until age 7-8.
Gender-Related Diagnostic Issues
1. Biological differences: Boys are more likely to experience nocturnal enuresis due to slower bladder development.
2. Societal expectations: Boys may be more stigmatized for enuresis, leading to underreporting or delayed seeking of treatment.
3. Diagnostic bias: Clinicians may be more likely to diagnose enuresis in boys due to stereotypes around male bedwetting.
4. Hormonal influences: Hormonal fluctuations during puberty can affect bladder control in girls, leading to misdiagnosis.
5. Pregnancy and childbirth: Women may experience enuresis during pregnancy or postpartum due to hormonal changes and pelvic floor trauma.
Examples
- Boys are 1.5-2 times more likely to experience nocturnal enuresis than girls.
- Girls are more likely to experience diurnal enuresis due to hormonal fluctuations during puberty.
- Women are more likely to experience enuresis during pregnancy and postpartum due to hormonal changes and pelvic floor trauma.
The negative impact of Enuresis on life
The negative impact of Enuresis (Bedwetting) on life can be significant and far-reaching, affecting various aspects of an individual's life, including:
1. Emotional Distress: Feelings of shame, guilt, anxiety, and low self-esteem.
2. Social Isolation: Avoidance of social activities, sleepovers, and overnight trips due to fear of accidents.
3. Sleep Disturbances: Difficulty sleeping, insomnia, or daytime fatigue due to nighttime awakenings.
4. Self-Esteem and Confidence: Negative impact on self-image, confidence, and overall well-being.
5. Relationships: Strained relationships with family members, caregivers, or peers due to frustration, anger, or embarrassment.
6. Daily Life: Restrictions on daily activities, such as avoiding long trips or social events, due to fear of accidents.
7. Mental Health: Increased risk of developing mental health conditions, such as depression, anxiety disorders, or attention deficit hyperactivity disorder (ADHD).
8. Physical Health: Skin irritation, urinary tract infections, or other medical complications due to prolonged exposure to urine.
9. Financial Burden: Increased costs for laundry, cleaning supplies, and medical treatment.
10. Quality of Life: Reduced overall quality of life, impacting daily functioning, happiness, and well-being.
In children, Enuresis can also lead to
1. Delayed Development: Delayed emotional, social, and cognitive development due to shame, anxiety, or low self-esteem.
2. Behavioral Problems: Increased risk of behavioral problems, such as attention deficit hyperactivity disorder (ADHD) or oppositional defiant disorder (ODD).
3. School Performance: Poor academic performance or absenteeism due to shame, anxiety, or sleep disturbances.
In adults, Enuresis can lead to
1. Career and Education: Impact on career advancement, education, or social opportunities due to shame, anxiety, or sleep disturbances.
2. Intimate Relationships: Strained intimate relationships due to feelings of shame
Differential Diagnosis
1. Urinary Tract Infections (UTIs): UTIs can cause frequent urination, urgency, and accidents.
2. Diabetes Mellitus: Uncontrolled diabetes can lead to increased urine production and accidents.
3. Neurological Disorders: Conditions like spina bifida, cerebral palsy, or multiple sclerosis can affect bladder control.
4. Sleep Disorders: Sleep apnea, restless leg syndrome, or insomnia can increase the likelihood of bedwetting.
5. Constipation: Constipation can cause urinary retention, leading to accidents.
6. Medication Side Effects: Certain medications, such as sedatives or diuretics, can increase urine production.
7. Anatomical Abnormalities: Abnormalities in the urinary tract, such as a small bladder or urethral obstruction, can cause enuresis.
8. Hormonal Imbalances: Hormonal changes during puberty or menopause can affect bladder control.
9. Psychological Factors: Anxiety, depression, or stress can contribute to enuresis.
10. Developmental Delays: Children with developmental delays may experience enuresis due to delayed bladder control.
Other conditions that may be considered in the differential diagnosis of enuresis include:
1. Overactive Bladder: Characterized by frequent urination, urgency, and accidents.
2. Detrusor Overactivity: A condition where the bladder muscle contracts too frequently, leading to accidents.
3. Vesicoureteral Reflux: A condition where urine flows backward from the bladder to the kidneys, increasing the risk of UTIs.
4. Bladder Outlet Obstruction: A blockage in the urethra or bladder neck that can cause urinary retention and accidents.
A comprehensive evaluation, including
1. Medical history
2. Physical examination
3. Urinal
Comorbidity
1. Attention Deficit Hyperactivity Disorder (ADHD): Studies suggest that 10-20% of children with ADHD also experience enuresis.
2. Anxiety Disorders: Anxiety can exacerbate enuresis, and 20-30% of children with enuresis also experience anxiety disorders.
3. Depression: Depression can co-occur with enuresis, particularly in older children and adults.
4. Sleep Disorders: Sleep apnea, restless leg syndrome, and other sleep disorders can contribute to enuresis.
5. Constipation: Constipation can cause urinary retention, leading to enuresis.
6. Urinary Tract Infections (UTIs): UTIs can cause enuresis, particularly in girls.
7. Neurodevelopmental Disorders: Conditions like autism spectrum disorder, Down syndrome, and cerebral palsy can increase the risk of enuresis.
8. Sleep-Related Breathing Disorders: Sleep-related breathing disorders, such as sleep apnea, can contribute to enuresis.
9. Gastroesophageal Reflux Disease (GERD): GERD can cause discomfort during sleep, leading to enuresis.
10. Neurological Disorders: Conditions like spina bifida, hydrocephalus, and neurodegenerative disorders can affect bladder control and lead to enuresis.
Comorbidities can impact the treatment and management of enuresis. A comprehensive evaluation by a healthcare professional is essential to identify and address any underlying conditions.
In addition to these comorbidities, enuresis can also have a significant impact on daily life, causing:
- Emotional distress and shame
- Social isolation and avoidance of social activities
- Decreased self-esteem and confidence
- Sleep disturbances and fatigue
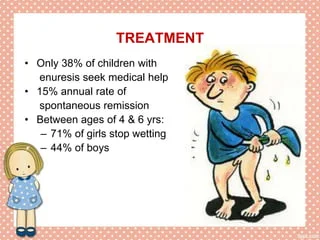
Treatment and Management
Behavioral Therapies
1. Bedwetting Alarms: Devices that detect moisture and alert the individual to wake up and use the bathroom.
2. Scheduled Waking: Waking the individual at regular intervals to use the bathroom.
3. Bladder Training: Gradually increasing the time between bathroom visits to help the bladder learn to hold urine.
4. Positive Reinforcement: Rewarding the individual for dry nights or successful use of the bathroom.
Medical Treatments
1. Desmopressin: A medication that reduces urine production at night.
2. Anticholinergics: Medications that help relax the bladder muscle and increase bladder capacity.
3. Imipramine: An antidepressant that can help with bedwetting, but is usually used as a last resort.
Lifestyle Changes
1. Fluid Management: Limiting fluids before bedtime and encouraging regular drinking during the day.
2. Dietary Changes: Avoid bladder irritants like caffeine, sugar, and spicy foods.
3. Bowel Habits: Encouraging regular bowel movements to prevent constipation.
4. Sleep Habits: Establishing a consistent sleep schedule and creating a relaxing bedtime routine.
Alternative Therapies
1. Acupuncture: This may help improve bladder control and reduce bedwetting.
2. Hypnotherapy: This may help the individual relax and gain control over their bladder.
3. Biofeedback Therapy: This may help the individual become aware of their bladder sensations and learn to control them.
Management
1. Protective Gear: Using mattress protectors, underwear, and pants to minimize accidents.
2. Emotional Support: Providing reassurance and support to help the individual cope with the emotional impact of bedwetting.