Restless Legs Syndrome (RLS) is a neurological disorder characterized by an uncontrollable urge to move one's legs, usually due to uncomfortable or unpleasant sensations. These sensations can occur during rest, relaxation, or inactivity, and are relieved by movement. Follow us here at Nightmare Disorder
Diagnostic Criteria for Restless Legs Syndrome
1. Urge to move the legs: An uncontrollable urge to move the legs, usually due to uncomfortable sensations.
2. Uncomfortable sensations: Sensations can be described as creeping, crawling, tingling, burning, or aching.
3. Worsening at rest: Symptoms worsen during rest, relaxation, or inactivity.
4. Relief with movement: Symptoms are relieved by movement, such as walking or stretching.
5. Worsening in the evening or night: Symptoms worsen in the evening or night, disrupting sleep.
6. No other condition explains the symptoms: RLS is not better explained by another medical or neurological condition.
Related: Rapid Eye Movement Sleep Behavior Disorder
Related: Non-Rapid Eye Movement (NREM) Sleep Arousal Disorders
Related: Circadian Rhythm Sleep-Wake Disorders (CRSWDs)
Related: Breathing-related sleep disorder
Related:
Hypersomnolence Disorder
Supportive Criteria
1. Family history: Family history of RLS.
2. Periodic limb movements during sleep: Periodic limb movements during sleep (PLMS) are common in RLS.
3. dopamine response: Symptoms may respond to dopamine agonists or levodopa.
The International Restless Legs Syndrome Study Group (IRLSSG) provides the diagnostic criteria for RLS.
Signs and Symptoms
Signs and Symptoms of Restless Legs Syndrome (RLS):
Common Symptoms
1. Urge to move: Uncontrollable urge to move the legs, usually due to uncomfortable sensations.
2. Uncomfortable sensations: Creeping, crawling, tingling, burning, or aching sensations in the legs.
3. Restlessness: Feeling of restlessness or agitation in the legs.
4. Relief with movement: Symptoms relieved by movement, such as walking or stretching.
5. Worsening at rest: Symptoms worsen during rest, relaxation, or inactivity.
6. Nighttime symptoms: Symptoms worsen in the evening or night, disrupting sleep.
Other Symptoms
1. Periodic limb movements: Periodic limb movements during sleep (PLMS) or while awake.
2. Sleep disturbances: Insomnia, daytime fatigue, or sleepiness.
3. Anxiety and stress: Anxiety, stress, or irritability due to symptoms.
4. Depression: Depression or mood disturbances.
5. Difficulty concentrating: Difficulty concentrating or paying attention.
Physical Signs
1. Leg twitching: Twitching or jerking of the legs.
2. Foot tapping: Tapping or shaking of the feet.
3. Leg stretching: Stretching or flexing of the legs.
4. Pacing: Pacing or walking due to restlessness.
Severity
1. Mild: Symptoms occur occasionally, with minimal impact on daily life.
2. Moderate: Symptoms occur regularly, with some impact on daily life.
3. Severe: Symptoms occur frequently, with a significant impact on daily life.
Associative Features
Associative Features of Restless Legs Syndrome (RLS):
Common Associative Features
1. Periodic Limb Movement Disorder (PLMD): PLMD is a common associate of RLS, characterized by periodic limb movements during sleep or wakefulness.
2. Sleep Disturbances: Insomnia, daytime fatigue, sleepiness, and restless sleep are common associates of RLS.
3. Pain Conditions: Fibromyalgia, arthritis, and other pain conditions often co-occur with RLS.
4. Anxiety and Depression: Anxiety, depression, and mood disturbances are common associates of RLS.
5. Attention Deficit Hyperactivity Disorder (ADHD): ADHD often co-occurs with RLS, particularly in children and adolescents.
6. Autonomic Dysfunction: Autonomic dysfunction, such as orthostatic intolerance, may be associated with RLS.
7. Gastrointestinal Issues: Gastrointestinal issues, such as irritable bowel syndrome (IBS), may be associated with RLS.
8. Hormonal Changes: Hormonal changes, such as those experienced during pregnancy or menopause, may trigger or worsen RLS.
9. Nutritional Deficiencies: Nutritional deficiencies, such as iron, magnesium, or vitamin B12 deficiency, may contribute to RLS.
10. Other Medical Conditions: Certain medical conditions, such as kidney disease, diabetes, and peripheral neuropathy, may be associated with RLS.
Less Common Associative Features
1. Parkinson's Disease: RLS may be an early symptom of Parkinson's disease.
2. Multiple System Atrophy: RLS may be associated with multiple system atrophy.
3. Friedreich's Ataxia: RLS may be associated with Friedreich's ataxia.
4. Charcot-Marie-Tooth Disease: RLS may be associated with Charcot-Marie-Tooth disease.
Ways to Diagnose Restless Legs Syndrome
Ways to Diagnose Restless Legs Syndrome (RLS):
1. Medical History: Comprehensive medical history to identify symptoms, family history, and other medical conditions.
2. Physical Examination: Physical examination to rule out other conditions that may cause similar symptoms.
3. Diagnostic Criteria: Use of the International Restless Legs Syndrome Study Group (IRLSSG) diagnostic criteria:
- Urge to move the legs
- Uncomfortable sensations
- Worsening at rest
- Relief with movement
- Worsening in the evening or night
4. Sleep Study: Polysomnography (PSG) or home sleep testing to assess sleep disturbances and periodic limb movements.
5. Blood Tests: Blood tests to rule out underlying medical conditions, such as:
- Iron deficiency
- Kidney disease
- Diabetes
- Peripheral neuropathy
6. Neurological Examination: Neurological examination to assess for:
- Peripheral neuropathy
- Parkinson's disease
- Other neurological conditions
7. Questionnaires and Scales: Use of questionnaires and scales, such as:
- International Restless Legs Syndrome Rating Scale (IRLS)
- Restless Legs Syndrome Quality of Life (RLS-QOL) questionnaire
8. Genetic Testing: Genetic testing for familial RLS or associated genetic conditions.
9. Imaging Studies: Imaging studies, such as MRI or CT scans, to rule out underlying structural abnormalities.
10. Differential Diagnosis: Differential diagnosis to rule out other conditions that may cause similar symptoms, such as:
- Periodic limb movement disorder
- Sleep apnea
- Narcolepsy
- Fibromyalgia
Prevalence and Demographics
Prevalence and Demographics of Restless Legs Syndrome (RLS):
Prevalence
Estimated to affect 7-10% of the general population
Affects approximately 12 million people in the United States
More common in:
- Women (1.5-2 times more likely than men)
- Older adults (prevalence increases with age)
- Caucasians (more common than African Americans or Asians)
Demographics
Age:
- Typically begins between 20-40 years old
- Peaks in prevalence between 40-60 years old
Gender:
- Women: 10-15% prevalence
- Men: 5-10% prevalence
Ethnicity:
- Caucasians: 10-15% prevalence
- African Americans: 5-10% prevalence
- Asians: 2-5% prevalence
Family History:
- 30-50% of people with RLS have a family history
- Increased risk if a first-degree relative is affected
Development and Course
Development and Course of Restless Legs Syndrome (RLS):
Early Development
RLS can start at any age, even in childhood
Early symptoms may be mild and intermittent
May be triggered by:
- Hormonal changes (pregnancy, menopause)
- Sleep disturbances
- Stress
- Certain medications
Progression
Symptoms can worsen over time
The frequency and severity of episodes may increase
May become more resistant to treatment
This can lead to:
- Sleep disturbances
- Fatigue
- Depression
- Anxiety
- Impaired quality of life
Course
RLS can follow a variable course:
- Some people experience mild and infrequent symptoms
- Others experience severe and frequent symptoms
Symptoms can:
- Wax and wane
- Change in severity and frequency
- Be influenced by lifestyle factors (sleep, exercise, stress)
Can be divided into:
- Early-onset RLS (before age 45)
- Late-onset RLS (after age 45)
Late-onset RLS tends to be more severe and progressive
Complications
Sleep disturbances
Fatigue
Depression
Anxiety
Impaired quality of life
Increased risk of:
- Cardiovascular disease
- Diabetes
- Hypertension
Etiology and Prognostic factors
Etiology of Restless Legs Syndrome (RLS):
Genetic Factors
- Family history: 30-50% of people with RLS have a family history
- Genetic mutations: MEIS1, BTBD9, and MAP2K5 genes
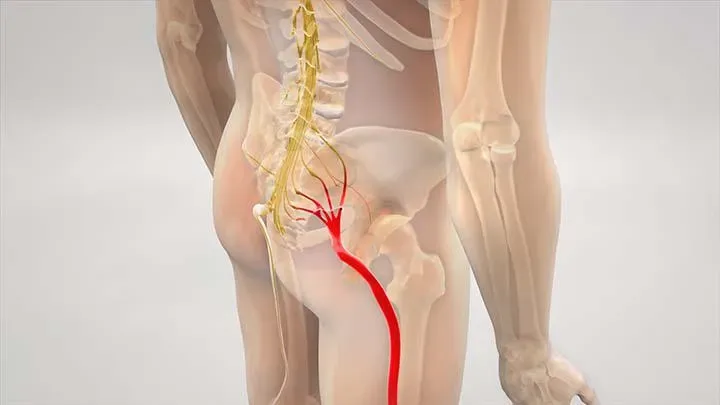
Neurological Factors
- Dopamine dysfunction: Imbalance in dopamine pathways
- Iron deficiency: Low iron levels in the brain
- Brain iron deposition: Abnormal iron deposition in the brain
Environmental Factors
- Sleep disturbances: Sleep deprivation, sleep apnea
- Stress: Physical or emotional stress
- Hormonal changes: Pregnancy, menopause
- Medications: Certain antidepressants, antihistamines
Other Factors
- Kidney disease
- Diabetes
- Peripheral neuropathy
- Parkinson's disease
Prognostic Factors of RLS
Good Prognostic Factors
- Early diagnosis and treatment
- Mild symptoms
- No family history
- No comorbidities
Poor Prognostic Factors
- Late diagnosis and treatment
- Severe symptoms
- Family history
- Comorbidities (kidney disease, diabetes, etc.)
- Presence of periodic limb movements during sleep
Neutral Prognostic Factors
- Age of onset
- Gender
- Ethnicity
Causes in Daily Life
Causes of Restless Legs Syndrome (RLS) in Daily Life:
1. Lack of physical activity: A sedentary lifestyle can trigger RLS symptoms.
2. Poor sleep habits: Irregular sleep schedule, sleep deprivation, or sleep disorders like sleep apnea.
3. Stress and anxiety: Physical or emotional stress can exacerbate RLS symptoms.
4. Caffeine and nicotine: Consuming caffeine and nicotine, especially in large amounts.
5. Alcohol: Excessive alcohol consumption can trigger RLS symptoms.
6. Medications: Certain antidepressants, antihistamines, and antipsychotics can cause RLS.
7. Prolonged sitting or standing: Remaining in one position for extended periods.
8. Travel: Long trips, especially by car or plane, can trigger RLS symptoms.
9. Hormonal changes: Pregnancy, menopause, or hormonal fluctuations.
10. Nutritional deficiencies: Low levels of iron, magnesium, or vitamin B12.
11. Dehydration: Not drinking enough water or losing fluids.
12. Medical conditions: Kidney disease, diabetes, peripheral neuropathy, or Parkinson's disease.
13. Aging: RLS symptoms can worsen with age.
14. Genetic predisposition: Family history of RLS.
15. Environmental factors: Exposure to toxins, heavy metals, or certain chemicals.
Gender-Related Diagnostic Issues
Gender-Related Diagnostic Issues of Restless Legs Syndrome (RLS):
1. Underdiagnosis in women: RLS is often misdiagnosed as anxiety, depression, or hormonal imbalances in women.
2. Overdiagnosis in men: RLS may be overdiagnosed in men due to a higher index of suspicion.
3. Hormonal influences: Fluctuating hormones during pregnancy, menstruation, and menopause can affect RLS symptoms.
4. Pregnancy: RLS symptoms often emerge or worsen during pregnancy, especially in the third trimester.
5. Menopause: RLS symptoms may increase during menopause due to hormonal changes.
Diagnostic Markers
Diagnostic Markers of RLS:
1. Clinical history: Detailed medical history, including symptoms, family history, and sleep patterns.
2. Physical examination: Neurological examination to rule out other conditions.
3. Sleep study: Polysomnography (PSG) or home sleep testing to assess sleep disturbances.
4. Blood tests: Iron, ferritin, magnesium, and vitamin B12 levels to rule out deficiencies.
5. Genetic testing: Genetic mutations associated with RLS, such as MEIS1, BTBD9, and MAP2K5.
6. Imaging studies: MRI or CT scans to rule out structural abnormalities.
7. Questionnaires and scales: International Restless Legs Syndrome Rating Scale (IRLS) and Restless Legs Syndrome Quality of Life (RLS-QOL) questionnaire.
8. Actigraphy: Wearable devices to monitor movement and activity patterns.
9. Electromyography (EMG): To assess muscle activity during sleep.
10. Periodic limb movement index (PLMI): To quantify periodic limb movements during sleep.
Negative Impacts of Restless Legs Syndrome on Life
Negative Impacts of Restless Legs Syndrome (RLS) on Life:
1. Sleep Disturbances: RLS disrupts sleep patterns, leading to insomnia, daytime fatigue, and sleepiness.
2. Mood Disturbances: RLS is associated with depression, anxiety, irritability, and mood swings.
3. Impaired Quality of Life: RLS affects daily activities, social relationships, and overall well-being.
4. Pain and Discomfort: RLS causes uncomfortable sensations, pain, and cramping in the legs.
5. Fatigue and Weakness: RLS leads to physical and mental exhaustion.
6. Concentration and Memory Problems: RLS affects attention, concentration, and memory.
7. Social Isolation: RLS may lead to avoidance of social activities due to embarrassment or discomfort.
8. Relationship Strains: RLS can affect relationships with family and friends due to irritability, mood swings, and sleep disturbances.
9. Work-Related Problems: RLS can impact job performance, attendance, and overall career advancement.
10. Mental Health Concerns: RLS increases the risk of developing mental health conditions like depression and anxiety disorders.
11. Reduced Productivity: RLS affects daily productivity, hobbies, and interests.
12. Increased Healthcare Utilization: RLS leads to increased healthcare visits, tests, and treatments.
13. Economic Burden: RLS imposes significant economic burdens on individuals and society.
14. Reduced Travel and Leisure Activities: RLS may limit travel and leisure activities due to discomfort and sleep disturbances.
15. Stigma and Embarrassment: RLS can lead to feelings of stigma and embarrassment, affecting self-esteem and confidence.
Differential Diagnosis
Differential Diagnosis of Restless Legs Syndrome (RLS) involves considering other conditions that may present with similar symptoms, such as:
1. Leg cramps: Painful muscle contractions, often occurring at night.
2. Fibromyalgia: Widespread muscle pain and tenderness.
3. Neuropathic pain: Pain due to nerve damage or dysfunction.
4. Peripheral artery disease: Leg pain due to reduced blood flow.
5. Sleep apnea: Pauses in breathing during sleep, leading to disrupted sleep.
6. Narcolepsy: Excessive daytime sleepiness, cataplexy, and sleep paralysis.
7. Parkinson's disease: Neurodegenerative disorder causing motor symptoms.
8. Multiple system atrophy: Neurodegenerative disorder causing motor and autonomic symptoms.
9. Friedreich's ataxia: Genetic disorder causing progressive damage to the nervous system.
10. Charcot-Marie-Tooth disease: Genetic disorder causing peripheral nerve damage.
11. Diabetic neuropathy: Nerve damage due to diabetes.
12. Hypokalemic periodic paralysis: Muscle weakness and cramps due to low potassium levels.
13. Muscle cramps: Painful muscle contractions, often occurring at night.
14. Nocturnal leg cramps: Painful muscle contractions occurring at night.
15. Sleep-related leg cramps: Painful muscle contractions during sleep.
To differentiate RLS from these conditions, a comprehensive diagnostic evaluation is necessary, including:
- Medical history
- Physical examination
- Sleep studies (e.g., polysomnography, actigraphy)
- Laboratory tests (e.g., iron, ferritin, magnesium, vitamin B12 levels)
- Imaging studies (e.g., MRI, CT scans)
- Questionnaires and scales (e.g., International Restless Legs Syndrome Rating Scale)
Comorbidity
What is comorbidity?
Comorbidity refers to the presence of one or more additional health conditions alongside a primary condition, in this case, RLS.
Types of comorbidity
1. Psychiatric comorbidity: RLS often co-occurs with mental health conditions like depression, anxiety, and ADHD.
2. Medical comorbidity: RLS can co-exist with other medical conditions like diabetes, hypertension, and sleep disorders.
3. Neurological comorbidity: RLS can occur alongside other neurological conditions like Parkinson's disease, peripheral neuropathy, and multiple system atrophy.
Factors contributing to comorbidity
1. Shared risk factors: Common risk factors like genetics, lifestyle, and environmental factors can contribute to both RLS and comorbid conditions.
2. Overlapping symptoms: Similar symptoms can make diagnosis and treatment challenging.
3. Complex pathophysiology: RLS and comorbid conditions can share underlying pathophysiological mechanisms.
Impact of comorbidity
1. Diagnosis: Comorbidity can make diagnosis more challenging.
2. Treatment: Comorbidity requires adjustments to treatment plans.
3. Prognosis: Comorbidity can affect disease severity and progression.
4. Quality of life: Comorbidity can impair daily functioning and well-being.
Managing comorbidity
1. Integrated care: Collaborative care between healthcare professionals.
2. Personalized treatment: Tailoring treatment plans to individual needs.
3. Lifestyle modifications: Encouraging healthy lifestyle habits.
4. Monitoring: Regular monitoring of symptoms and treatment effectiveness.
Treatment and Management
RLS is a chronic condition that requires a comprehensive treatment approach. The goal of treatment is to manage symptoms, improve sleep quality, and enhance overall quality of life.
Non-Pharmacological Interventions
1. Lifestyle Modifications
Regular exercise: Regular physical activity can help reduce RLS symptoms.
Balanced diet: A healthy diet rich in essential nutrients, vitamins, and minerals can help alleviate symptoms.
Stress management: Stress can exacerbate RLS symptoms.
Relaxation techniques: Techniques like progressive muscle relaxation, visualization, and mindfulness can help manage stress and reduce symptoms.
2. Sleep Hygiene
Establish a consistent sleep schedule: Irregular sleep patterns can worsen RLS symptoms.
Create a relaxing sleep environment: Make your bedroom a sleep haven by ensuring it is dark, quiet, and cool.
Avoid caffeine, nicotine, and electronics before bedtime: These can disrupt sleep patterns and worsen RLS symptoms.
3. Alternative Therapies
Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body to stimulate healing and relaxation.
Massage therapy: Massage can help reduce muscle tension, promote relaxation, and improve sleep quality.
Physical therapy: A physical therapist can help you develop a personalized exercise program to manage RLS symptoms.\
Pharmacological Interventions:
1. Dopaminergic Agents
Dopamine agonists (e.g., ropinirole, pramipexole): These medications mimic dopamine's effects in the brain, helping to reduce symptoms.
Levodopa: This medication increases dopamine levels in the brain, providing relief from symptoms.
2. Opioids
Oxycodone: This medication can help manage pain and discomfort associated with RLS.
Hydrocodone: This medication can help alleviate pain and reduce symptoms.
3. Benzodiazepines
Clonazepam: This medication can help manage anxiety, insomnia, and restlessness associated with RLS.
Diazepam: This medication can help reduce muscle spasms, anxiety, and insomnia.
4. Anticonvulsants
Gabapentin: This medication can help manage pain, anxiety, and insomnia associated with RLS.
Pregabalin: This medication can help reduce pain, anxiety, and insomnia.
5. Iron Supplements
Iron-deficiency RLS: Iron supplements can help alleviate symptoms in individuals with iron-deficiency RLS.
Other Treatments
1. Transcutaneous Electrical Nerve Stimulation (TENS):
- TENS involves applying electrical impulses to the skin to manage pain and discomfort.
2. Vibratory Stimulation:
- Vibratory stimulation involves applying vibrations to the skin to reduce symptoms.
3. Botulinum Toxin Injections:
- Botulinum toxin injections can help manage severe RLS symptoms by relaxing muscles.
Management Strategies
1. Regular Follow-up:
- Regular follow-up appointments with your healthcare provider can help monitor symptoms, adjust treatment plans, and address comorbidities.
2. Adjust Treatment Plans:
- Treatment plans may need to be adjusted based on symptom severity, response to treatment, and changes in lifestyle or health status.
3. Patient Education:
- Educating patients on RLS, treatment options, and lifestyle modifications can help them take an active role in managing their symptoms.
4. Multidisciplinary Care:
- Collaborating with healthcare professionals from various disciplines can help address comorbidities, optimize treatment, and improve overall care.
By combining non-pharmacological interventions, pharmacological treatments, and management strategies, individuals with RLS can effectively manage their symptoms, improve sleep quality, and enhance their overall quality of life.