The repeated regurgitation of food characterizes rumination disorder after eating. This regurgitated food is then often re-chewed and either swallowed again or spit out. Unlike vomiting, it typically occurs without nausea or effort.
It's important to note that rumination disorder is distinct from bulimia nervosa, as there's no binge eating or purging behavior involved.
This condition can affect individuals of all ages, though it's more commonly recognized in infants and people with developmental disabilities. Follow us here at Blake Lively & Gigi Hadid
Criteria
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), the criteria for rumination disorder are as follows:
- Repeated regurgitation of food for at least one month.
- The regurgitated food may be re-chewed, re-swallowed, or spit out.
- The eating disorder must not occur only in the presence of anorexia nervosa, bulimia nervosa, binge eating disorder, or avoidant/restrictive food intake disorder.
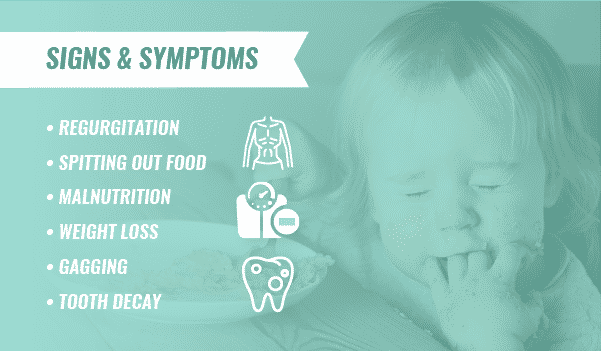
Signs & Symptoms
The primary symptom of rumination disorder is the *repeated regurgitation of food* without effort or nausea. Other associated signs and symptoms include:
- Discomfort or pain: Abdominal pain or bloating may occur.
- Weight loss: Due to reduced food intake or nutritional deficiencies.
- Dental problems: Tooth decay or bad breath can develop from constant exposure to stomach acid.
- Social isolation: Embarrassment about the condition can lead to social withdrawal.
- Malnutrition: If severe, can lead to nutritional deficiencies.
Causes
The exact causes of rumination disorder are not fully understood, but several factors may contribute:
- Developmental factors: Issues with feeding or swallowing in infancy may play a role.
- Psychological factors: Underlying emotional or psychological problems, such as anxiety or depression, could contribute.
- Medical conditions: Gastrointestinal disorders or neurological conditions might be associated with rumination.
Associative Features
Rumination disorder is often associated with:
- Developmental or intellectual disabilities: It's more common in individuals with these conditions.
- Other eating disorders: While not a diagnostic criterion, it can coexist with other eating disorders.
- Psychological conditions: Depression, anxiety, or social isolation may be present.
Prevalence and Demographics
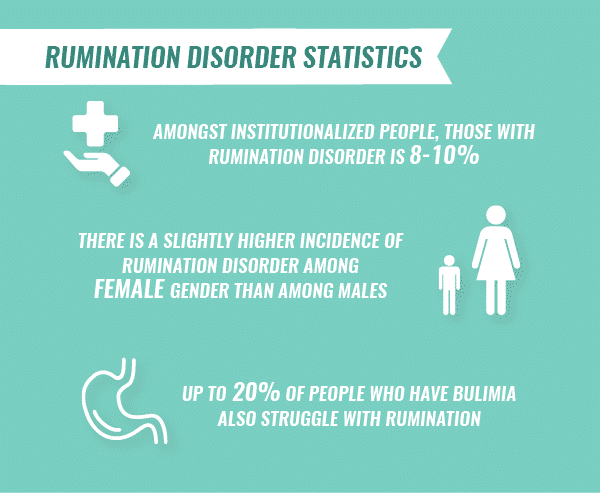
Prevalence
Rumination disorder is relatively rare. Due to underreporting and the challenges in diagnosing the condition, specific prevalence rates are limited. However, it is more commonly observed in:
- Infants and young children: This age group is most frequently affected.
- Individuals with intellectual or developmental disabilities: These individuals have a higher prevalence of rumination disorder.
Demographics
- Age: The disorder typically begins in infancy or early childhood.
- Gender: While there is limited data, some studies suggest a slightly higher prevalence in males.
- Geographic location: Prevalence rates may vary across different regions and cultures.
Development and Course
Development
The exact cause of rumination disorder is unknown, but several factors are implicated:
- Infant development: It often appears in infants and young children, possibly due to lack of stimulation or abnormal mother-infant bonding.
- Psychological factors: Stress, anxiety, or underlying emotional issues may contribute to the development of rumination in older children and adults.
- Medical conditions: In some cases, underlying medical conditions can contribute to the disorder.
Course
The course of rumination disorder can vary widely:
- Onset: It typically starts in infancy or early childhood but can occur at any age.
- Duration: The disorder can be episodic or chronic.
- Severity: Symptoms can range from mild to severe, affecting daily life and nutrition.
- Remission: In some cases, particularly in infants, the disorder may resolve spontaneously.
Risk Factors and Prognostic Factors
Risk Factors
- Infancy or childhood: The disorder is more common in this age group.
- Developmental disabilities: Individuals with intellectual or developmental disabilities are at higher risk.
- Psychological conditions: Existing mental health issues can increase the risk.
Prognostic Factors
Factors that may influence the course and outcome of rumination disorder include:
- Early intervention: Prompt diagnosis and treatment can improve prognosis.
- Severity of symptoms: The severity of rumination can impact the treatment process.
- Underlying medical conditions: Other health issues may influence treatment outcomes.
- Family support: A supportive environment can aid in recovery.
Impact on Life
Rumination disorder can have a significant impact on an individual's life, affecting physical, emotional, and social well-being.
- Physical impact: Malnutrition, dehydration, dental problems, and growth retardation in children.
- Psychological impact: Low self-esteem, body image issues, anxiety, depression, and social isolation.
- Social impact: Difficulty maintaining relationships due to embarrassment or social withdrawal.
Complications of Rumination Disorder
- Malnutrition and growth failure, especially in children.
- Electrolyte imbalances.
- Dental problems due to exposure to stomach acid.
- Skin problems.
- Social and emotional difficulties.
Functional Consequences
Rumination disorder can significantly impact an individual's quality of life. Some of the functional consequences include:
Physical health
- Malnutrition due to inadequate food intake
- Weight loss
- Dental problems due to exposure to stomach acid
- Dehydration
- Electrolyte imbalances
Psychological impact
- Low self-esteem
- Body image issues
- Social isolation due to embarrassment
- Anxiety and depression
Social and occupational difficulties
- Challenges in maintaining relationships or employment due to the condition.
Differential Diagnosis
It's crucial to distinguish rumination disorder from other conditions to ensure accurate diagnosis and appropriate treatment.
Gastrointestinal Conditions
- Gastroesophageal reflux disease (GERD): Often involves heartburn and chest pain, which are typically absent in rumination disorder.
- Pyloric stenosis: Obstruction of the stomach outlet, usually seen in infants.
- Hiatal hernia: Part of the stomach bulges through the diaphragm, often causing heartburn.
- Gastroparesis: Delayed stomach emptying, leading to nausea, vomiting, and bloating.
- Other gastrointestinal disorders: Conditions like esophagitis, gastritis, or peptic ulcer disease can cause similar symptoms.
Eating Disorders
- Bulimia nervosa: Involves binge eating followed by purging, unlike rumination disorder.
Neurological Conditions
- Dysphagia: Difficulty swallowing.
- Gastrointestinal motility disorders: Issues with the muscles of the digestive system.
Comorbidity
Rumination disorder often co-occurs with other conditions, which can complicate diagnosis and treatment. Some common comorbidities include:
- Intellectual disability: Individuals with intellectual disabilities are at higher risk for rumination disorder.
- Autism spectrum disorder: There is an association between rumination and autism.
- Other eating disorders: While not a diagnostic criterion, it can coexist with other eating disorders like anorexia nervosa or bulimia nervosa.
- Gastrointestinal disorders: Conditions like gastroesophageal reflux disease (GERD) may be present.
- Psychological disorders: Depression, anxiety, and attention deficit hyperactivity disorder (ADHD) can sometimes be associated with rumination disorder.
Diagnosis of Rumination Disorder
Diagnosis of rumination disorder is primarily based on clinical evaluation and observation of the patient's behavior.
- Key factors in diagnosis:
- A detailed medical history, including dietary habits, bowel movements, and any associated symptoms.
- Observation of the regurgitation process.
Treatment and Management
Treatment for rumination disorder primarily focuses on behavioral therapy and addressing any underlying medical or psychological conditions.
Behavioral Therapy
- Diaphragmatic breathing: This is a key component of treatment, as it helps to relax the abdominal muscles and prevent regurgitation.
- Postural changes: Maintaining an upright posture after meals can help reduce the likelihood of regurgitation.
- Mealtime routines: Establishing consistent meal times and a calm eating environment can be beneficial.
- Distraction techniques: Engaging in activities that distract from the urge to regurgitate.
Medical Management
- Medications: While there's no specific medication for rumination disorder, medications might be prescribed to address associated conditions, such as acid reflux or depression.
- Nutritional support: In severe cases, nutritional supplements or tube feeding may be necessary.
Additional Considerations
- Family involvement: Involving caregivers in the treatment process is essential, especially for children.
- Underlying conditions: Addressing any associated medical or psychological conditions is crucial for successful treatment.
- Patience and consistency: Treatment may take time, and consistent application of therapy techniques is important.