Depression, also known as Major Depressive Disorder (MDD), affects millions worldwide. It's a leading cause of disability, impacting daily life, relationships, and overall well-being.
Depression is a complex mental health disorder characterized by persistent feelings of sadness, hopelessness, and loss of interest in activities. Follow us here at How to Perform Mindfulness-Based Cognitive Therapy.
Subtypes of Depression
1. Major Depressive Disorder (MDD): The most common type, characterized by persistent depressive symptoms.
2. Dysthymia (Persistent Depressive Disorder): Long-term, low-grade depression lasting 2+ years.
3. Postpartum Depression (PPD): Depression following childbirth, affects mothers and fathers.
4. Seasonal Affective Disorder (SAD): Depression related to seasonal changes, typically winter.
5. Bipolar Disorder: Manic-depressive illness, alternating between depression and mania.
6. Atypical Depression: Uncommon subtype, characterized by improved mood in response to positive events.
7. Melancholic Depression: Severe depression with loss of pleasure in activities.
8. Psychotic Depression: Depression with hallucinations or delusions.
9. Somatic Depression: Physical symptoms predominate, such as pain or fatigue.
10. Adjustment Disorder with Depressed Mood: Depression following significant life changes.
Related: What is Solution-Focused Brief Therapy (SFBT)
Related: What is Psychodynamic Therapy?
Signs and symptoms of all subtypes of depression
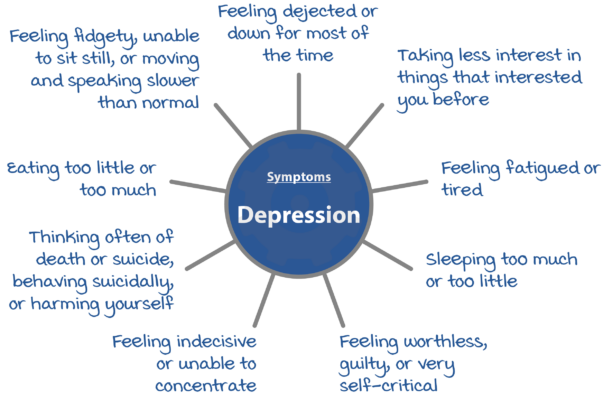
Here are the signs and symptoms of various subtypes of depression:
1. Major Depressive Disorder (MDD)
- Persistent feelings of sadness, emptiness, or hopelessness
- Loss of interest in activities once enjoyed
- Changes in appetite or sleep patterns
- Fatigue or low-energy
- Difficulty concentrating or making decisions
- Feelings of guilt, worthlessness, or helplessness
- Social withdrawal
- Physical symptoms (e.g., headaches, pain)
2. Dysthymia (Persistent Depressive Disorder)
- Low-grade depression lasting 2+ years
- Persistent feelings of sadness or hopelessness
- Loss of interest in activities
- Changes in appetite or sleep patterns
- Fatigue or low-energy
- Difficulty concentrating
- Feelings of guilt or worthlessness
- Social withdrawal
3. Postpartum Depression (PPD)
- Onset within 4 weeks post-delivery
- Feelings of sadness, hopelessness, or anxiety
- Mood swings
- Difficulty bonding with baby
- Changes in appetite or sleep patterns
- Fatigue or low-energy
- Irritability or anger
- Feelings of guilt or shame
4. Seasonal Affective Disorder (SAD)
- Depression during winter months
- Feelings of sadness, lethargy, or hopelessness
- Social withdrawal
- Changes in appetite (cravings for carbohydrates)
- Sleep patterns disrupted (hypersomnia)
- Fatigue or low-energy
- Weight gain
5. Bipolar Disorder
- Manic episodes (elevated mood, increased energy)
- Depressive episodes (sadness, hopelessness)
- Mood swings
- Irritability or anger
- Impulsive behavior
- Changes in sleep patterns
- Grandiose thoughts or behaviors
6. Atypical Depression
- Improved mood in response to positive events
- Weight gain or increased appetite
- Hypersomnia (excessive sleep)
- Lead paralysis (heavy or leaden feeling in arms/legs)
- Sensitivity to rejection
- Social anxiety
7. Melancholic Depression
- Loss of pleasure in activities
- Significant weight loss or loss of appetite
- Insomnia or hypersomnia
- Psychomotor agitation or retardation
- Feelings of guilt or worthlessness
- Suicidal thoughts or behaviors
8. Psychotic Depression
- Hallucinations (hearing/seeing things not present)
- Delusions (false beliefs)
- Disorganized thinking or behavior
- Negative symptoms (apathy, flat affect)
- Suicidal thoughts or behaviors
- Social withdrawal
9. Somatic Depression
- Physical symptoms predominate (pain, fatigue, headaches)
- Changes in appetite or sleep patterns
- Difficulty concentrating
- Feelings of guilt or worthlessness
- Social withdrawal
- Irritability or anger
10. Adjustment Disorder with Depressed Mood
- Depression following significant life changes (divorce, job loss)
- Feelings of sadness or hopelessness
- Changes in appetite or sleep patterns
- Fatigue or low-energy
- Difficulty concentrating
- Social withdrawal
Other Subtypes
- Premenstrual Dysphoric Disorder (PMDD): Depression, anxiety, and irritability during the premenstrual phase.
- Depressive Disorder Not Otherwise Specified (DD-NOS): Depression that doesn't meet criteria for other subtypes.
Keep in mind that everyone experiences depression differently, and not everyone will exhibit all symptoms.
Common Causes and Risk Factors
1. Genetics: Family history of depression
2. Brain chemistry: Imbalance of neurotransmitters (e.g., serotonin, dopamine)
3. Life events: Trauma, stress, loss, significant changes
4. Medical conditions: Chronic illness, pain, disability
5. Substance abuse: Alcohol, drugs, or medication misuse
6. Social and environmental factors: Social isolation, poverty, lack of support
Subtype-Specific Causes and Risk Factors
Major Depressive Disorder (MDD)
1. Genetic predisposition
2. Brain chemistry imbalance
3. Life events (e.g., trauma, loss)
4. Medical conditions (e.g., chronic pain)
5. Substance abuse
Dysthymia (Persistent Depressive Disorder)
1. Childhood trauma or neglect
2. Family history of depression
3. Brain chemistry imbalance
4. Chronic stress
5. Social isolation
Postpartum Depression (PPD)
1. Hormonal changes post-childbirth
2. History of depression or anxiety
3. Traumatic childbirth experience
4. Lack of social support
5. Previous history of PPD
Seasonal Affective Disorder (SAD)
1. Geographic location (far from the equator)
2. Lack of sunlight exposure
3. Genetic predisposition
4. Hormonal changes (e.g., melatonin)
5. Previous history of SAD
Bipolar Disorder
1. Genetic predisposition
2. Brain chemistry imbalance
3. Life events (e.g., trauma, stress)
4. Substance abuse
5. Family history of bipolar disorder
Atypical Depression
1. Childhood trauma or neglect
2. Family history of depression
3. Brain chemistry imbalance
4. Social anxiety
5. Previous history of atypical depression
Melancholic Depression
1. Genetic predisposition
2. Brain chemistry imbalance
3. Life events (e.g., trauma, loss)
4. Medical conditions (e.g., chronic pain)
5. Substance abuse
Psychotic Depression
1. Family history of psychotic disorders
2. Brain chemistry imbalance
3. Life events (e.g., trauma, stress)
4. Substance abuse
5. Previous history of psychotic episodes
Somatic Depression
1. Chronic medical conditions (e.g., pain, disability)
2. Substance abuse
3. Life events (e.g., trauma, loss)
4. Brain chemistry imbalance
5. Family history of depression
Adjustment Disorder with Depressed Mood
1. Significant life changes (e.g., divorce, job loss)
2. Lack of social support
3. Previous history of adjustment disorders
4. Brain chemistry imbalance
5. Substance abuse
Other Factors
1. Age: Depression can affect anyone, but risk increases with age
2. Gender: Women are more likely to experience depression
3. Socioeconomic status: Poverty, lack of access to healthcare
4. Cultural background: Cultural and social factors influencing mental health
Keep in mind that depression is complex, and multiple factors contribute to its development.
Step-by-step Guide for Diagnosing depression and its subtypes
Diagnosing depression and its subtypes involves a comprehensive evaluation:
Step 1: Initial Assessment
1. Clinical interview: Patient's history, symptoms, and concerns.
2. Physical examination: Ruling out underlying medical conditions.
3. Psychiatric history: Previous mental health diagnoses, and treatments.
Step 2: Diagnostic Criteria
1. Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria.
2. International Classification of Diseases (ICD-10) criteria.
Step 3: Symptom Evaluation
1. Mood symptoms: Sadness, hopelessness, loss of interest.
2. Cognitive symptoms: Difficulty concentrating, and decision-making.
3. Physical symptoms: Changes in appetite, sleep, energy.
4. Behavioral symptoms: Social withdrawal, irritability.
Step 4: Subtype Identification
1. Major Depressive Disorder (MDD): 5+ symptoms, 2+ weeks.
2. Dysthymia: Low-grade depression, 2+ years.
3. Postpartum Depression (PPD): Onset within 4 weeks post-delivery.
4. Seasonal Affective Disorder (SAD): Depression during winter months.
5. Bipolar Disorder: Manic/hypomanic episodes.
6. Atypical Depression: Improved mood with positive events.
7. Melancholic Depression: Loss of pleasure, significant weight loss.
8. Psychotic Depression: Hallucinations, delusions.
Step 5: Rating Scales and Questionnaires
1. Patient Health Questionnaire (PHQ-9)
2. Beck Depression Inventory (BDI)
3. Hamilton Rating Scale for Depression (HAM-D)
4. Montgomery-Åsberg Depression Rating Scale (MADRS)
Step 6: Differential Diagnosis
1. Rule out other mental health conditions (e.g., anxiety, PTSD).
2. Consider medical conditions (e.g., hypothyroidism, chronic pain).
3. Substance abuse or medication-induced depression.
Step 7: Comprehensive Diagnostic Evaluation
1. Combine clinical interview, diagnostic criteria, and symptom evaluation.
2. Consider rating scales and questionnaires.
3. Consult with other healthcare professionals (e.g., psychologists, psychiatrists).
Diagnostic Tools
1. DSM-5
2. ICD-10
3. PHQ-9
4. BDI
5. HAM-D
6. MADRS
7. Clinical interview guides (e.g., SCID, MINI)
Special Considerations
1. Children and adolescents: Consider the developmental stage.
2. Older adults: Consider cognitive decline and medical conditions.
3. Cultural and linguistic diversity: Consider cultural influences.
Accurate Diagnosis
1. Essential for effective treatment.
2. Prevents misdiagnosis and inappropriate treatment.
3. Enhances patient outcomes and quality of life.
Treatment and management
Treatment and management of depression typically involve a combination of:
Psychotherapies
1. Cognitive-Behavioral Therapy (CBT): Helps change negative thought patterns.
2. Interpersonal Therapy (IPT): Focuses on relationships and communication.
3. Psychodynamic Therapy: Explores underlying emotional conflicts.
4. Dialectical Behavior Therapy (DBT): Combines CBT with mindfulness techniques.
5. Mindfulness-Based Cognitive Therapy (MBCT): Prevents relapse.
Medications
1. Selective Serotonin Reuptake Inhibitors (SSRIs): Fluoxetine (Prozac), sertraline (Zoloft).
2. Serotonin-norepinephrine reuptake Inhibitors (SNRIs): Venlafaxine (Effexor), duloxetine (Cymbalta).
3. Tricyclic Antidepressants (TCAs): Amitriptyline (Elavil), imipramine (Tofranil).
4. Monoamine Oxidase Inhibitors (MAOIs): Phenelzine (Nardil), tranylcypromine (Parnate).
5. Atypical Antidepressants: Bupropion (Wellbutrin), mirtazapine (Remeron).
Lifestyle Changes
1. Regular exercise: Improves mood, and reduces symptoms.
2. Healthy diet: Balanced nutrition supports mental health.
3. Sleep hygiene: Establishes consistent sleep patterns.
4. Stress management: Techniques like meditation, and yoga.
5. Social support: Building and maintaining relationships.
Alternative Therapies
1. Herbal supplements: St. John's Wort, omega-3 fatty acids.
2. Acupuncture: This may help alleviate symptoms.
3. Mindfulness-based interventions: Mindfulness-Based Stress Reduction (MBSR).
4. Eye movement desensitization and reprocessing (EMDR): For trauma-related depression.
Hospitalization and Emergency Care
1. Severe symptoms: Suicidal thoughts, psychotic episodes.
2. Acute treatment: Stabilization, medication adjustment.
3. Intensive outpatient programs: Structured therapy and support.
Self-Help Strategies
1. Journaling: Expressing emotions, and tracking progress.
2. Support groups: Connecting with others experiencing depression.
3. Online resources: Educational websites, forums.
4. Mobile apps: Mood-tracking, mindfulness exercises.
Prevention
1. Early intervention: Addressing symptoms promptly.
2. Maintenance therapy: Continuing treatment to prevent relapse.
3. Lifestyle modifications: Regular exercise, healthy diet.
4. Stress management: Developing coping strategies.
Treatment-Resistant Depression
1. Combination therapy: Multiple medications or therapies.
2. Augmentation therapy: Adding medications or therapies.
3. Electroconvulsive Therapy (ECT): For severe, treatment-resistant cases.
4. Transcranial Magnetic Stimulation (TMS): Non-invasive brain stimulation.
Special Considerations
1. Children and adolescents: Family-based therapy, medication.
2. Older adults: Age-specific considerations, medication management.
3. Pregnancy and postpartum: Safe medication options, therapy.
4. Cultural and linguistic diversity: Culturally sensitive treatment.